Michael Rotman, MD, FRCPC, PhD | Medically reviewed by Robin Backlund, BHSc Last update:
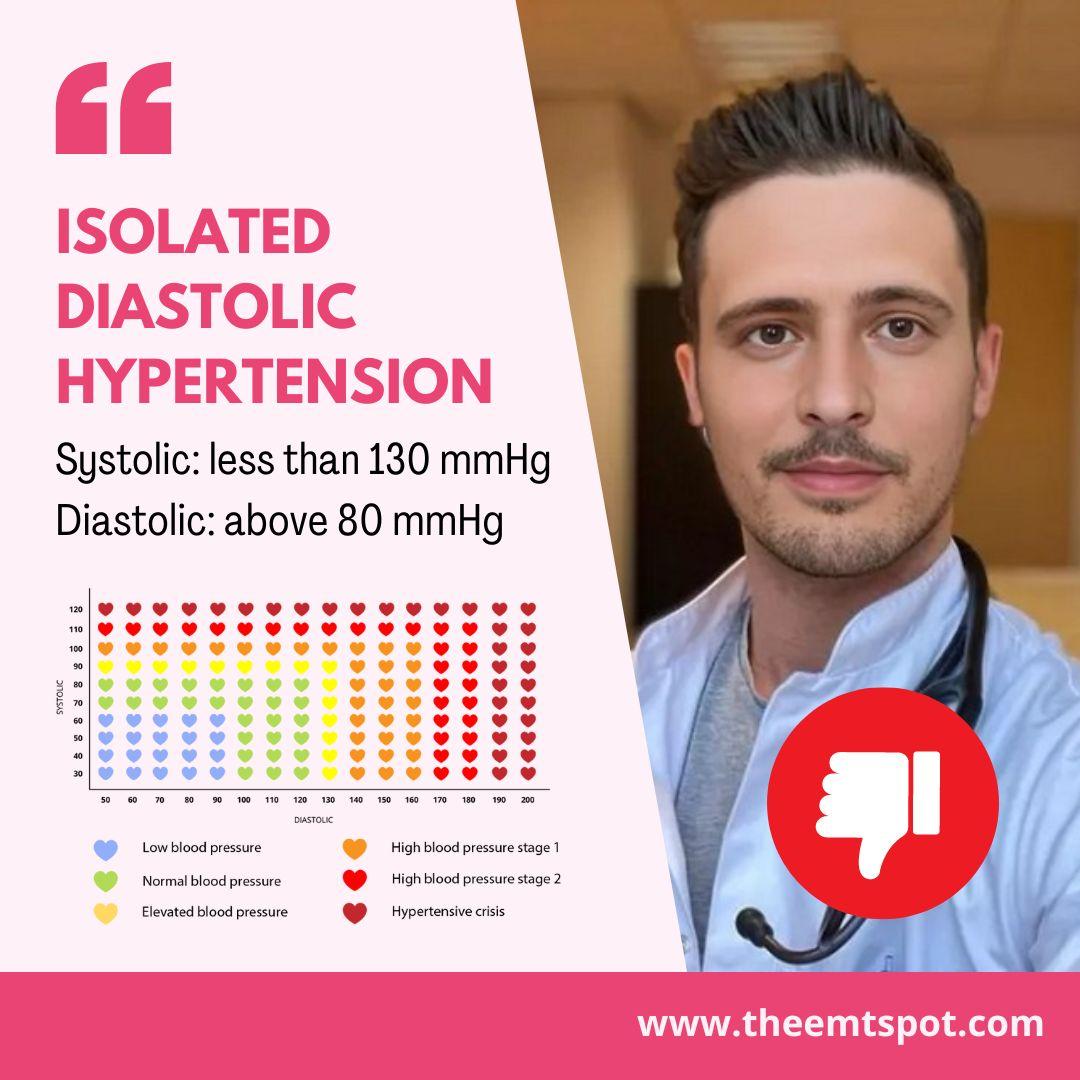
What is isolated diastolic hypertension (IDH)?
IDH is an early indicator of potential cardiovascular disease affecting the heart and kidneys.
Bạn đang xem: Blood Pressure 119/86 mmHg: What Does It Indicate?
Understanding IDH is vital for preserving cardiovascular health, particularly considering its distinct characteristics and implications for long-term well-being.
While a single reading of 119/86 mmHg may not necessarily indicate IDH, consistently falling within the range described below raises concerns.
While ACC/AHA determines IDH to be a DBP higher than 80 mmHg with SBP less than 130 mmHg, the European Society of Cardiology (ESC) begs to differ.
According to ESC, a DBP higher than 90 mmHg with a SBP less than 140 mmHg is considered IDH.
Either way, A 2020 study published in JAMA Journal by Dr. McEvoy and colleagues reports that in the US alone, 1.3 – 6.5% of people suffer from IDH, which is a concerning figure.
IDH often goes unnoticed due to its subtle presentation; however, its recognition is essential for preventing potential cardiovascular complications.
It’s particularly prevalent among younger adults and can signify an increased risk of developing more pronounced hypertension in the future. Monitoring blood pressure regularly is vital for early detection and management.
The condition also poses a risk to the vascular system, contributing to the development of atherosclerosis (hardening of the arteries), which can further elevate the risk of stroke and peripheral artery disease.
Doctors utilize IDH data to pinpoint individuals at higher cardiovascular risk, even with normal systolic pressure.
IDH signals the potential for future hypertension and organ damage, guiding personalized treatment and monitoring. It enables early interventions, tailoring of treatments, and adjustments over time to prevent serious health complications.
Moreover, the understanding of IDH’s impact on health is evolving. Ongoing research continues to shed light on its implications and the best practices for management.
Xem thêm : How To Eat 200 Grams of Protein A Day: 5-Day Sample Meal Plans
This highlights the significance of remaining well-informed and seeking guidance from healthcare professionals for tailored advice and treatment plans.
But how would you identify if you have IDH? Read the section below, and it will help you identify a few of the associated symptoms, even though it is mostly asymptomatic.
What are the symptoms of isolated diastolic hypertension?
IDH is clinically asymptomatic in most cases; however, some individuals with 119/86 mmHg might experience subtle signs indicative of elevated diastolic blood pressure or related complications.
Below are some potential symptoms and associated signs according to Dr. Rohini Radhakrishnan’s medical write-up on MedicineNet.
- Mild to severe headaches: Occasional headaches may become more frequent or intense due to the heightened pressure on the blood vessels in the brain.
- Dizziness or lightheadedness: Fluctuations in blood pressure can cause moments of dizziness, particularly when standing up quickly from a sitting or lying position.
- Palpitations: Experiencing a fast or irregular heartbeat may occasionally indicate IDH, as the heart exerts more effort to circulate blood against elevated diastolic pressure.
- Fatigue: Unexplained tiredness or a general feeling of being unwell could be related to IDH, as the body’s organs might not receive an optimal blood supply.
- Blurred vision: Elevated diastolic blood pressure has the potential to impact the blood vessels within the eyes, resulting in temporary disruptions to vision.
- Shortness of breath: In some cases, especially when IDH has led to heart-related issues, individuals may experience difficulty breathing during physical activity or even at rest.
- Nosebleeds: Though less common, sudden and unexplained nosebleeds can occur in people with significantly elevated blood pressure levels.
- Chest pain: In severe cases, especially if IDH contributes to heart disease, chest pain or discomfort may manifest, signaling a potential heart problem.
It’s important to recognize that many of these symptoms can be nonspecific and attributed to a variety of health issues.
Identifying and addressing IDH early is key to preventing potential complications and maintaining overall health.
But you need to know what has happened in order to treat the root cause. Read further to learn more about the causes of IDH, which can help you eliminate it from the root.
What are the causes of isolated diastolic hypertension?
IDH arises from a complex interplay of various factors, and understanding its causes is essential for effective management.
According to a medically reviewed article by Irmanie Hemphill, MD, FAAFP below are the primary causes and contributing factors.
- Age-related changes: Younger individuals are more likely to develop IDH due to the relative elasticity of their arterial walls, which can more easily accommodate high diastolic pressure.
- Lifestyle factors: Unhealthy lifestyle habits like consuming a high-sodium diet, being inactive, excessive alcohol intake, and smoking can play a role in causing IDH.
- Genetic predisposition: A family history of hypertension increases the likelihood of developing IDH, indicating a genetic component to the condition.
- Obesity: Excess body weight is strongly linked to increased blood pressure, including diastolic pressure, due to the added strain on the heart and arteries.
- High cholesterol: Elevated levels of bad cholesterol (LDL) can lead to atherosclerosis, which can stiffen the arteries and affect diastolic blood pressure.
- Diabetes: This condition can damage the arteries, making them more susceptible to hypertension, including IDH.
- Kidney disease: The kidneys play a crucial role in regulating blood pressure, and damage to these organs can lead to various forms of hypertension.
- Endocrine disorders: Certain disorders affecting the glands that produce hormones, including IDH, can influence blood pressure.
- Medications: Certain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), specific antidepressants, and decongestants, have the potential to increase diastolic blood pressure.
Now that you know the symptoms and causes of IDH, gaining insight into the risks and dangers will enhance your understanding of IDH.
What are the risks and dangers associated with isolated diastolic hypertension?
An IDH of 119/86 mmHg poses several risks and dangers due to its impact on the cardiovascular system and other organs. Even though it involves only elevated diastolic pressure, the condition should not be taken lightly.
An article published by Yuichiro Yano in the AHA journal Hypertension in 2022 elaborates on some of the critical risks and dangers associated with IDH. Below is a list of them.
- Heart disease: IDH elevates the likelihood of developing coronary artery disease, which may lead to angina (chest pain), myocardial infarction (heart attack), and other cardiac issues.
- Stroke: Increased diastolic blood pressure can contribute to the development of blood clots or atherosclerosis in the arteries supplying the brain, thereby raising the likelihood of stroke.
- Kidney damage: The kidneys are highly vascular organs, and IDH can lead to nephropathy by damaging the blood vessels in the kidneys, potentially resulting in chronic kidney disease or kidney failure.
- Cognitive decline: High diastolic pressure can affect cerebral blood flow, contributing to cognitive decline, including impaired memory and executive function, and increasing the risk of dementia.
- Heart failure: IDH can result in heart failure by impeding the heart’s ability to pump blood effectively, ultimately causing the heart muscle to weaken over time.
- Peripheral artery disease: This condition, characterized by narrowed arteries in the legs, can be exacerbated by IDH, leading to reduced blood flow, pain, and mobility issues.
- Vision loss: The blood vessels in the eyes can be damaged by high blood pressure, leading to retinopathy, which can cause vision impairment or blindness.
Understanding these risks underscores the importance of managing IDH effectively to prevent these potentially severe health complications.
Xem thêm : Urinary tract infection
Some of the common treatment approaches involve regular monitoring, lifestyle changes, and, when necessary, medication, which can help mitigate the dangers associated with IDH. Check the next section to learn about it.
How do you treat isolated diastolic hypertension?
IDH can only be treated through a multifaceted approach for effective management. Lifestyle modification, medication, and constant monitoring are the three effective ways to manage an IDH of 119/86 mmHg.
Lifestyle modification
This includes adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins while limiting sodium intake.
Regular physical activity, such as aerobic exercises and strength training, can also help lower blood pressure.
Additionally, quitting smoking and moderating alcohol consumption are essential steps in managing IDH.
Medication
It may be necessary for some individuals with levels in the range of 119/86 mmHg.
Prof. P. Ginelli and J.N. Bella, in their 2012 publication in Nutrition, Metabolism, and Cardiovascular Diseases, compiled a list of clinical approaches for treating IDH.
According to them, antihypertensive medications, such as diuretics, ACE inhibitors, beta-blockers, or calcium channel blockers, may be prescribed by doctors to help control blood pressure levels.
Blood pressure monitoring
Regular blood pressure monitoring and consultation with your doctor are crucial for assessing treatment effectiveness and adjusting medication dosages as needed.
For clinically accurate results, you may consider top-of-the-line blood pressure monitors like Oxiline Pressure X Pro, CheckMe BP2, Omron Silver, or Withings BPM Connect.
It’s important to recognize that treating IDH is not just about lowering diastolic blood pressure but also addressing underlying risk factors to reduce the risk of cardiovascular complications such as heart disease, stroke, and kidney damage.
Nguồn: https://buycookiesonline.eu
Danh mục: Blog
This post was last modified on November 17, 2024 6:29 am