Since I worked in an ER for 25 years, I thought I had pretty much seen everything in medicine there was to see. But when I started working in jails, I was quickly confronted with clinical scenarios that I had no experience with from my ER days. Here is one such case:
- Risk of prostate cancer for men with prior negative biopsies undergoing magnetic resonance imaging compared with biopsy-naive men: A prospective evaluation of the PLUM cohort
- 8 Units of Safety 1St Alpha Omega Elite Air Car Seats (Expiration 2029/12/31) – MSRP 2400$ – Brand New (Lot # CP582302)
- AA Gill On…Being Assertive In Bed
- School Of Massage
- Creamy Mushroom and Black Beluga Lentil Stew
A 46-year-old man came into my jail medical clinic complaining of muscle aches and twitching, which he first noticed 2 days before. He had been booked into the jail 2 weeks previously. This patient’s currently prescribed medications prior to coming to jail were continued (as is our general policy): sertraline 200 mg a day, buspirone 15 mg PO BID, and trazodone 200 mg at bedtime. He also took lisinopril/hydrochlorothiazide and atorvastatin.
Bạn đang xem: Serotonin Fooled Me Once
The patient walked into clinic with an odd stiff-legged gait and a noticeable hand tremor. He had a heart rate of 124, a blood pressure of 156/100, and a temperature of 99.4° F. His speech was a bit anxious and pressured. Beads of sweat were visible on his forehead. His patellar reflex was exaggerated, but without clonus.
So, what was going on with this patient? I considered the “usual suspects,” such as infection, metabolic abnormalities (like hyperthyroidism), and methamphetamine intoxication (inmates can, indeed, sometimes get meth and other drugs despite being in jail). But I was most suspicious of serotonin syndrome – and this turned out to be the right diagnosis. Serotonin syndrome may be an uncommon or even rare condition in outside medicine (I had never seen a case in my ER career), but I have found it to be pretty common in jails.
Serotonin syndrome is a constellation of symptoms caused by an excess of the neurotransmitter serotonin. It ranges in severity from mild/moderate cases (like the one above) to fatal. Serotonin syndrome is characterized by a trinity of abnormalities:
1. Neuromuscular hyperactivity: muscle twitching, tremor, and hyperreflexia.
2. Autonomic effects: tachycardia, hypertension, hyperthermia, sweating, and shivering.
3. Mental status effects: anxiety, agitation, hypomania, confusion, and hallucinations.
Xem thêm : Chipotle Sour Cream Sauce
Mild cases of serotonin syndrome may only manifest as tremor, hyperreflexia, tachycardia, and sweating.
Moderately severe patients will additionally have an increased temperature, clonus, and agitation.
Patients with severe serotonin syndrome are typically delirious, hallucinating, and have very high temperatures (sometimes over 106° F), which can lead to all sorts of bad effects, like rhabdomyolysis, seizures, renal failure, and yes, death.
Serotonin syndrome is caused by drugs that increase serotonin levels in the brain. These are mostly psychiatric drugs, of course. The big three categories of serotonergic drugs are:
1. Selective serotonin reuptake inhibitors (SSRIs). My patient was taking sertraline (Zoloft), but don’t forget fluoxetine (Prozac), citalopram (Celexa), and many others.
2.Tricyclic antidepressants (TCAs), which act by blocking serotonin reuptake as well as norepinephrine reuptake. The ones I see used most are amitriptyline, imipramine, and doxepin.
3. Serotonin-norepinephrine reuptake inhibitors (SNRIs). This group includes trazodone, venlafaxine (Effexor), duloxetine (Cymbalta), and others. My patient was also taking trazodone.
You should memorize that list! However, many other drugs increase serotonin levels besides those in the big three categories. Interesting examples include amphetamines, buspirone, tramadol, and the triptans. My patient was also taking buspirone.
Xem thêm : Fitness
Clinicians inadvertently cause serotonin syndrome in their patients in two main ways. The first is when they prescribe large doses of serotonin drugs, usually an SSRI. A psychiatrist friend of mine told me that when Prozac was first introduced, doctors used to commonly prescribe large doses, like 80 mg or even more a day. As a result, my friend says he used to see lots of mild/moderate cases of serotonin syndrome caused by large doses of Prozac alone. It is less common to see large doses of SSRIs used nowadays, since it has been pretty well established that patients get little, if any, additional benefit from SSRIs by using extra-large doses. However, I still see large doses of SSRIs prescribed in the community and, in fact, my patient was taking the maximum dose of sertraline.
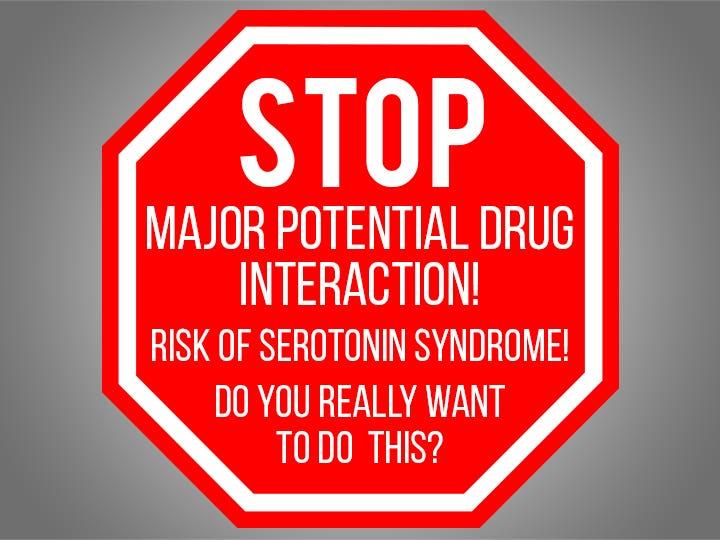
The second (and more important) cause of serotonin syndrome is when clinicians prescribe two or more different serotonin agents from two different categories. This practice is very common. For example, an SSRI is often prescribed along with trazodone for sleep. SSRIs are also combined with an SNRI or a TCA for severe depression. My patient was actually taking three serotonin drugs: sertraline, trazodone, and buspirone. I suspect that the practitioner in the community who prescribed all three did not check their drug interactions. If he had used the drug interaction checker that I generally use myself, a big red stop sign would have popped up saying (approximately): “Major potential drug interaction! Risk of serotonin syndrome! Do you really want to do this?”
Fortunately, my patient only had mild/moderate serotonin syndrome, so I was able to successfully treat him by stopping all three drugs and giving him a little diazepam. He was asymptomatic the next day. However, serotonin syndrome can manifest itself much more rapidly and be much more severe, as I had learned from an earlier patient.
This patient was a middle-aged man in jail who was prescribed both paroxetine (Paxil) and imipramine (Tofranil) by his outside psychiatrist. A couple of months after his incarceration, he developed agitation, hallucinations, vomiting and within several hours became unresponsive. At the ER, he had a temperature of 107° F, intense muscle rigidity, and full-blown shock. This case did not turn out well.
This tragic case occurred early in my correctional medicine career. It made me vigilant in looking for evidence of serotonin syndrome – and I subsequently have found several mild/moderate cases since. This case also made me question whether the benefit of combining two serotonergic agents in one patient ever outweighs the risk. I personally don’t believe so.
Whether you agree or disagree with this conclusion, please remember the danger of serotonin syndrome when you “max out” the dose of SSRIs or especially if you combine serotonergic agents. You may have used a particular combination like sertraline-trazodone a hundred times and have never seen ill effects, but that does not mean you never will! Consider carefully whether the benefits of combining serotonergic drugs truly outweigh the risk of serotonin syndrome.
Don’t get burned like I did!
Jeffrey E. Keller, MD, FACEP, is a board-certified emergency physician with 25 years of experience before moving full time into his “true calling” of correctional medicine. He now works exclusively in jails and prisons, and blogs about correctional medicine at JailMedicine.com.
Comment
Nguồn: https://buycookiesonline.eu
Danh mục: Info
This post was last modified on December 13, 2024 1:05 pm