Sedgwick County is coming off a summer COVID wave as it heads into cold and flu season.
- Quick Tip: Bench Press More Right Now
- Outcome of bone-patellar tendon-bone vs hamstring tendon autograft for anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials with a 5-year minimum follow-up
- Keto Sweetener Conversion Chart For Erythritol, Monk Fruit, Stevia, & More
- Dye Stealer Pregnancy Test: What Does it Mean?
Health officials hope that surge prompts far more people to sign up for the new COVID vaccine, which is recommended annually for people 6 months and older.
Bạn đang xem: COVID vaccines have arrived in Wichita. Here’s what else you need to stay healthy
Last year, the U.S. Centers for Disease Control and Prevention reported that fewer than a quarter of adults actually got the new COVID vaccine.
COVID viral activity levels remain high in Kansas, according to the CDC’s monitoring of wastewater.
But COVID is just one of the respiratory illnesses doctors worry about. Flu and respiratory syncytial virus, known as RSV, can be severe and even deadly for the very young and elderly.
Health officials stress the importance of the COVID and flu vaccines for most people, and the RSV vaccine for the elderly or pregnant people and young children.
Jump down to answers about when and where to get the vaccine and what it might cost you
Adrienne Byrne, director of Sedgwick County Health Department, said the slightly higher number of COVID cases this summer was unusual. Cases usually don’t peak until schools begin and then again during the winter holidays.
“We already began to see an increase (of COVID cases) before school started,” Byrne said. “It is important — as important as it always is — to get the updated flu and updated COVID vaccine.”
Doctors and health officials say the COVID vaccine is the best way to prevent serious illness. It also reduces the risk of developing long COVID, a debilitating condition where people experience symptoms for months or years.
After the federal government ended its public health emergency in May 2023, the vaccine price rose to over $100 — CVS charges more than $200.
People covered by Medicare, Medicaid and most private insurance can still get the shot for free or for a small fee. The $1 billion federal Bridge Access Program made free shots available to uninsured people, but it ran out of money at the end of August.
“We’re not going to refuse a vaccine to anyone,” Byrne said.
The end of that federal funding, Byrne said, means the health department will have fewer COVID vaccines for people with insurance.
Kansas got $780,000 from the federal government to buy COVID vaccines. The state is working with county health officials to determine demand. Jill Bronaugh, spokesperson for the Kansas Department of Health and Environment, said the shots will be “equitably distributed” across the state.
Each year, Wichita Public Schools offers flu vaccine clinics for its students. Kimber Kasitz, the district’s director of health services, said Wichita schools educate students about the importance of prevention and vaccines.
“We really try to push preventative measures,” Kasitz said, “like getting the shots ahead of time, as soon as they come out.”
Xem thêm : How Long Do Canned Sardines Last Once Opened?
The school district also provides a free combo test to students, which tests for flu A, flu B and COVID and tracks positive cases
Wichita Public Schools is experiencing a “small surge” of COVID cases, Kasitz said. The district works closely with the Sedgwick County Health Department and follows its recommendations for increasing precautions.
The schools follow the CDC guidelines, with students and staff required to be fever-free for at least 24 hours before returning. Students can receive their work through email or Teams.
“We certainly don’t want people coming to work if they can’t function in their role because they don’t feel well,” Kasitz said. “A student too, because that’s just going to make it last longer if you push yourself too quickly.”
Where can I get the new COVID vaccine and how much will it cost?
Many pharmacies offer the vaccine on a walk-in basis. Retail chains like Walgreens and CVS let you sign up through their websites. People covered by Medicare, Medicaid and many private insurance plans still can get the COVID shot for free, but you may have to pay an administration fee.
Uninsured and underinsured minors get the shot for free through a federal program known as Vaccines for Children.
Where can I get vaccinated if I don’t have insurance?
Sedgwick County Health Department will help fill this gap for Wichitans, providing free COVID and flu vaccines to people without insurance. Byrne said the federal funding won’t affect this initiative because it is supported by two state programs.
- This fall, Sedgwick County Health Department will offer both vaccine appointments and walk-ins on Thursdays at 1 p.m. at its main clinic, 2716 W. Central Ave., Wichita. People will need to pay an administrative charge, but with proof of income, it can slide to $2.
In addition to the Sedgwick County Health Department, people without insurance can get vaccinated at federally funded clinics or public health clinics.
- HealthCore Clinic, 2707 E. 21st St. N., Wichita, provides COVID-19 vaccines to anyone 6 months or older. People can schedule appointments or go to a walk-in clinic on Thursdays from 2 to 5 p.m. Updated Pfizer and Moderna shots are available.
- Hunter Health Clinic, 527 N. Grove, Wichita, and 2750 S. Roosevelt, Wichita, offers COVID-19 vaccines for patients and community members ages 5 and older and offers free COVID-19 tests.
- Guadalupe Clinic, 940 S. St. Francis Ave., and 2825 S. Hillside, Wichita, serves patients with no insurance and those living within 200% of the federal poverty level. Its patients can receive the flu vaccine at no cost.
- Wichita Public Schools and Sedgwick County Health Department will host no-cost flu clinics for students on Oct. 18, 19 and 21 from 8 a.m. to 4 p.m. at Alvin E. Morris Administrative Center, 903 S. Edgemoor St., Wichita. Appointments are required.
What are the differences among the COVID vaccines?
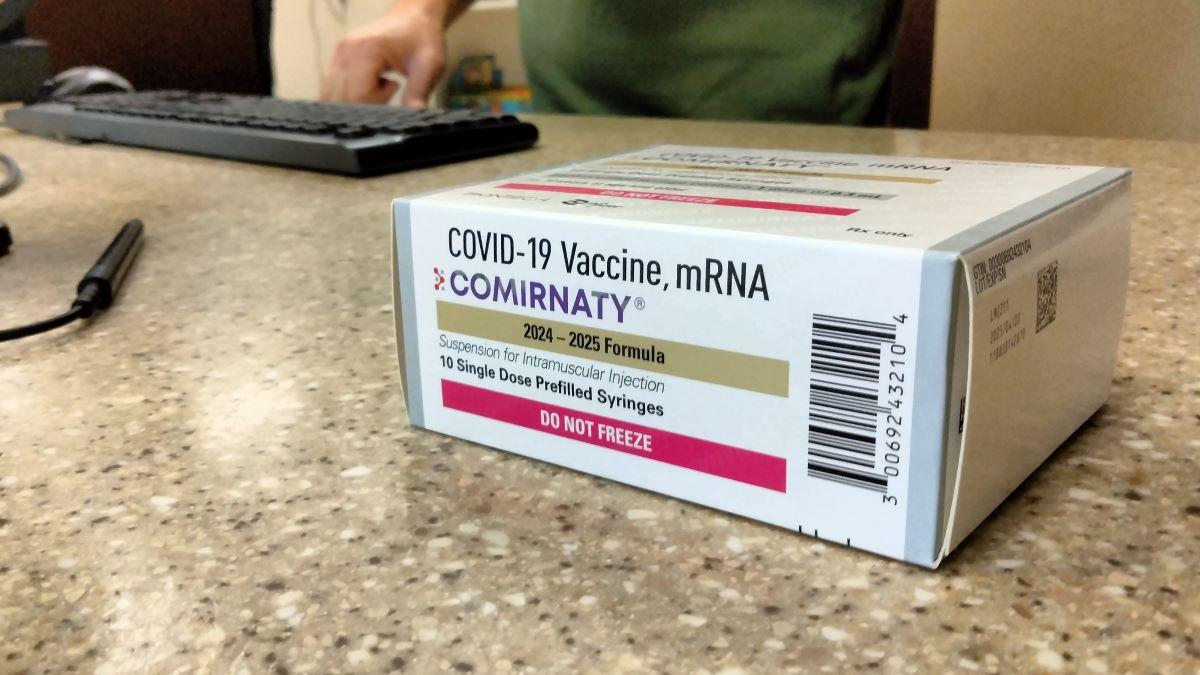
The U.S. Food and Drug Administration has fully approved the updated Pfizer, Moderna and Novavax vaccines.
The Pfizer and Moderna, both approved for anyone aged 6 months and older, use mRNA technology to help the body fight the virus causing COVID. Once injected, the mRNA instructs cells to make copies of spike proteins found on the virus, training the immune system to recognize and attack the real virus.
The Novavax vaccine, approved for those 12 years and older, is the only non-mRNA COVID vaccine available. It uses common vaccine technology to introduce a harmless version of the spike protein. The immune system recognizes it as foreign and produces antibodies, which will help protect against the actual virus.
What variants are the latest vaccines targeting?
The Moderna and Pfizer vaccines target the KP.2 strain of the virus. KP.2 is one of the FLiRT variants, the highly contagious versions of COVID that fueled this summer’s surge. Novavax specifically targets JN.1, but the company has reported that its vaccine protects against multiple variants, including KP.2 and KP.3.
What are the symptoms of the current COVID variants?
Many people infected with the current variants have reported symptoms similar to a cold or flu, said Dr. Amy Seery, a pediatrician for Ascension Via Christi Family Medicine Residency Program. That includes brain fog, fever, runny nose, coughing and muscle aches.
“So many people experienced a pretty nasty summer cold with our current wave, which we’ve determined was probably COVID,” she said.
The CDC reported that KP.3 has overtaken KP.2 as the dominant COVID-19 variant since June and estimated last month that its offshoot KP.3.1.1 has since become the dominant variant.
If I had COVID recently, how long should I wait to get the new COVID vaccine?
Doctors said you can wait up to three months after an infection to get the new vaccine. That’s because you will develop immunity from having the virus.
How long will the vaccine protect me?
Steele said you can expect the shot to keep you from getting sick for about three months. The vaccine will protect you from getting seriously ill for at least six months. Older adults and patients with underlying health conditions may be advised to get a second shot midway through the year.
If I get sick, when should I test?
Xem thêm : Birth Control
Test when you have symptoms, said Dr. Sarah Boyd, an infectious disease doctor at St. Luke’s Health System. And don’t assume you’re COVID-free if one home antigen test shows a negative result. When a cough, sore throat or other symptoms persist, you should test a second time 48 hours later to rule out COVID.
If I am exposed, when should I test?
If you know you’ve been exposed and you don’t have symptoms, you should test five days after exposure. Unless symptoms develop, you don’t need to repeat the test, Boyd said.
Where can I get COVID tests?
Beginning in late September, you will be able to order four free tests from the federal government. Tests are available to buy at most drug stores or online, but that can cost $6 a test or more. No-cost testing is still available at some pharmacies for people without insurance who have been exposed to COVID or have symptoms.
If the test is positive, do I need to stay home?
The CDC recommends that if you test positive, you should avoid contact with others. Once your symptoms are improving and you have been fever-free for 24 hours, you can go back to school or work — as long as you’re not returning to a health care setting. But when you go back into the world, you should take precautions like wearing a mask for five additional days.
Should I consider taking Paxlovid if I test positive?
It’s a good idea to check in with your doctor if you test positive, Boyd said. They may recommend that you take Paxlovid, an antiviral medication that can prevent serious illness. Testing and determining that you have COVID is especially important for people at higher risk because Paxlovid must be started within five days of getting sick.
How can I reduce my risks of getting long COVID?
The best strategy to avoid long COVID is to avoid being infected in the first place, experts said. Wear a mask in crowded places, practice good hand hygiene and avoid touching your eyes, nose and mouth when in public. Most importantly, stay up to date on the vaccine. Like the flu shot, updated COVID vaccines are tweaked to more closely match and repel the virus variants that are circulating.
Can I get the flu and COVID vaccines at the same time?
It is safe to get both the flu and COVID vaccines at the same time. Adults eligible for RSV vaccines can get all three together.
What are the symptoms of flu?
The main symptoms of flu are fever, cough, sore throat, runny or stuffy nose, muscle aches and fatigue.
Who should get the flu vaccine?
Flu season occurs in fall and winter, and vaccines also reduce the risk of severe illness. The CDC recommends a yearly flu vaccine for everyone 6 months and older, with September or October as the ideal time for vaccination.
An updated vaccine is important, Seery said, because like COVID, flu viruses continue to evolve.
“Having that updated vaccine can make a huge difference,” she said.
What are the symptoms of RSV?
RSV usually causes mild, coldlike symptoms, but infants and older adults are more likely to have a severe case and require hospitalization.
In 2023, the first two RSV vaccines licensed in the U.S. became available.
“As a pediatrician, I am very excited about RSV technology right now,” Seery said.
Who should get the RSV vaccine?
The CDC recommends one dose of the RSV vaccine for all adults aged 75 and older and for those 60-74 at risk of increased severe RSV disease. Adults can receive their RSV vaccine along with other vaccines, such as the flu and COVID vaccines.
Pregnant individuals can also receive vaccines to protect infants and young children from severe RSV. The vaccine allows the parent’s immune system to make antibodies that are passed down to the baby, providing it with extra protection for the first four to six months of life.
“This is just amazing for us because about 30% of children who get an RSV infection will require some level of elevated medical care … and that can be very scary for a parent, especially the younger the infant is,” Seery said.
If the parent doesn’t receive the RSV vaccine while pregnant, the CDC recommends that an infant is immunized with a monoclonal antibody that prevents severe RSV disease. This is also recommended for some children, aged 8 months to 19 months, who are at increased risk.
Nguồn: https://buycookiesonline.eu
Danh mục: Info
This post was last modified on December 2, 2024 12:16 pm