CataractDecember 2020
by Liz HillmanEditorial Co-Director
Cataract surgery anti-inflammatory regimens have changed significantly in the last decade, with an emphasis on improving patient compliance.
Bạn đang xem: Blog
“It has changed considerably; it’s changed in nuanced form and substance,” said Michael Saidel, MD “It’s changed in how we administer medications and which ones are available to us.”
Dr. Saidel said older forms of NSAIDs—ketorolac, diclofenac—have fallen away in his practice in favor of newer generation ones like bromfenac and nepafenac. He said he starts a patient on an NSAID 2 days preop and has them continue for several weeks postop.
“The big change has not been the drugs themselves but rather how I administer them,” Dr. Saidel said.
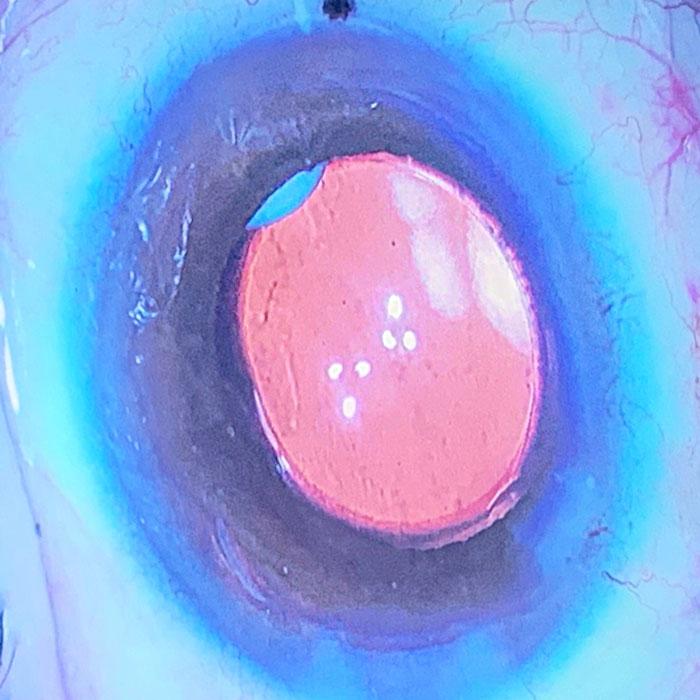
While topical has always been the most common, he said he’s now often using Dexycu (dexamethasone intraocular suspension 9%, EyePoint Pharmaceuticals) in many patients.
“I think it’s better to put the oil in the engine as opposed to pouring it on the engine,” he offered as an analogy.
Dr. Saidel said his use of corticosteroids has also evolved. He now uses a combination prednisolone/nepafenac/moxifloxacin instead of three different drops. He begins this 2 days preop and continues for a few weeks postop with standard TID dosing, no taper.
For Michael Savetsky, MD, changes in NSAID use over the past decade have been in frequency with a focus on patient compliance. When he started residency in 2008, he said three different eye drops—a steroid, antibiotic, and anti-inflammatory 4 times a day—were prescribed to cataract patients.
“As time went on, drug companies started coming out with new iterations of drops that you can use less frequently,” Dr. Savetsky said. “The biggest change started when doctors were attempting to go dropless, and that’s where we are right now.”
“In one surgery center, I’ve been injecting … moxifloxacin and Dexycu. Then [the patient goes] on an NSAID for 4 weeks once a day,” Dr. Savetsky said. “We have to confirm that insurance will cover the Dexycu, but it’s been convenient for patients when it goes through. At the other surgery center, I don’t have access to the moxifloxacin, so I will inject Dexycu—for those patients who are covered—and afterward the patient will take antibiotic and NSAID drops.”
Dr. Savetsky added that if there is a complication or if he anticipates more inflammation, he might put the patient on a steroid drop as well. Conversely, if the patient was a known steroid responder or had advanced glaucoma, he said he might not inject Dexycu.
Xem thêm : How Long Do Fillers Last? The Definitive Guide (Updated 2024)
Jeffrey Whitman, MD, said he injects a steroid and antibiotic into the vitreous or anterior chamber in about 40% of his patients. These include ones who he thinks might be more prone to inflammation, such as those with a history of iritis or uveitis, patients of African American or Hispanic descent who might have cell and flare longer, or those with a dense cataract where more ultrasound time might be required.
Dr. Whitman said he’s also using Dexycu more regularly now and noted that in 100+ cases, none have needed to use an additional steroid drop as a “rescue.” One downside to this option at the moment, Dr. Whitman said, is that despite its current pass-through status, some insurers are not accepting it, creating more work for the billing staff. Dr. Whitman also said his staff is looking at the rescue rate of Dexycu compared to Dextenza (dexamethasone ophthalmic insert 0.4 mg, Ocular Therapeutix).
“We’d like to use whatever is most successful in the eye. Also, all of these are steroids, not antibiotics, so you have to put the patient on an antibiotic as well,” he noted.
What hasn’t changed over the years are the reasons for using an NSAID. However, the literature conflicts as to whether one is necessary. A large, retrospective study by Modjtahedi et al. found that topical NSAIDs were associated with only a modest decrease in postoperative macular edema.1
“The risk for PME is low and the number of patients benefiting from treatment is small,” Modjtahedi et al wrote.
In contrast, the literature review by Hoffman et al. describes NSAIDs as “an important adjunctive tool for surgeons performing routine and complicated cataract surgery.”2
Dr. Savetsky said there are reasons other than CME prevention to use NSAIDs.
“If it prevents CME in more patients than not, it’s a nice additive,” Dr. Savetsky said. “I like the NSAID because I think they are particularly good at pain control versus corticosteroids. When you prescribe an NSAID and steroid, you then have a synergistic effect, where you hit two different areas of the inflammatory pathway.
“Prevention of miosis is another benefit, but mostly I think of pain and the synergy with a steroid,” he continued. “My objective is to get rid of the inflammation quickly, so the better I can do that, the better the comfort of the patients, and potentially a better outcome.”
Dr. Saidel also noted the benefit of NSAIDs for pain. “For me, that’s where NSAIDs shine in maintaining patient comfort,” he said.
Up until 10 years ago, Keith Walter, MD, was only using an NSAID without a steroid.
“I think we have seen that steroids alone aren’t the best answer to prevent CME. We need to have an NSAID on board to help prevent CME and lessen pain and inflammation,” Dr. Walter said.
Xem thêm : Low Dose Naltrexone: A New Frontier in the Battle Against Hair Loss
When Omidria (phenylephrine and ketorolac intraocular solution 1%/0.3%, Omeros) became available, Dr. Walter said he began using this combined with topical bromfenac. He found this combination allows him to achieve a “near zero CME rate.” Dr. Walter said that bromfenac specifically is the most potent at preventing CME when used properly for 30 days.
Why his push for reduced steroid use? Dr. Walter pointed out that ophthalmology is the only surgical specialty that puts steroids on a postop wound.
“Steroids delay wound healing, increase risk of infection, and, in our case, can cause a drastic rise in IOP,” he said. “Most studies comparing steroids and NSAIDs have concluded that the two together are ‘synergistic’ and should both be used, but they only include two arms in the study. One arm is steroids alone and the other is steroids plus an NSAIDs. What about the NSAID alone arm? It’s typically not there. So those studies are invalid, as I think that the ‘synergy’ is all from the NSAID.
“Some have claimed a steroid is needed for prevention of corneal edema,” Dr. Walter continued. “I find the data on this to be weak. When you look at all FDA studies where NSAIDs gain approval for postop cataract pain, the adverse events for corneal edema are less than 2% in the NSAID alone arm. My experience has been it doesn’t make any difference.”
Overall, when it comes to cataract anti-inflammatory regimens, Dr. Saidel said doctors need to consider several factors: cost, outcome, and patient ease and compliance.
“Cost reductions can be achieved using compounded drops. That is also something that will increase patient compliance. … In terms of administering the medication, whether in drop form or intraocular, you get fantastic patient compliance with intraocular injection of drugs. Because we know that patient compliance is so closely related to outcomes, that should be a strong motivator for any surgeon to consider providing that in their regimen.”
About the doctors
Michael Saidel, MDNorth Bay Eye AssociatesPetaluma, California
Michael Savetsky, MDSightMDNew York, New York
Keith Walter, MDWake Forest Baptist HealthWinston-Salem, North Carolina
Jeffrey Whitman, MDKey-Whitman Eye CenterDallas, Texas
References
- Modjtahedi BS, et al. Perioperative topical nonsteroidal anti-inflammatory drugs for macular edema prophylaxis following cataract surgery. Am J Ophthalmol. 2017;176:174-182.
- Hoffman RS, et al. Cataract surgery and nonsteroidal antiinflammatory drugs. J Cataract Refract Surg. 2016;42:1368-1379.
Relevant disclosures
Saidel: EyePoint Pharmaceuticals, Sun Pharma, Bausch + LombSavetsky: EyePoint Pharmaceuticals, Novartis, AllerganWalter: Omeros, Sun PharmaWhitman: None
Contact
Saidel: msaidel@yahoo.comSavetsky: msavetmd@gmail.comWalter: kwalter@wakehealth.eduWhitman: whitman@keywhitman.com
Nguồn: https://buycookiesonline.eu
Danh mục: Info
This post was last modified on December 7, 2024 7:07 am