In the United States, heart disease remains the number one cause of death across most groups and accounts for one in every four deaths.
Coronary Artery Disease (CAD) is the most common form of heart disease, affecting about 6.7% of adults aged over 20. Within CAD lies an extreme form, Triple Vessel Disease that affects a smaller number of patients.
Bạn đang xem: Blog
Here is how Triple Vessel Disease is identified and treated:
What is triple vessel disease?
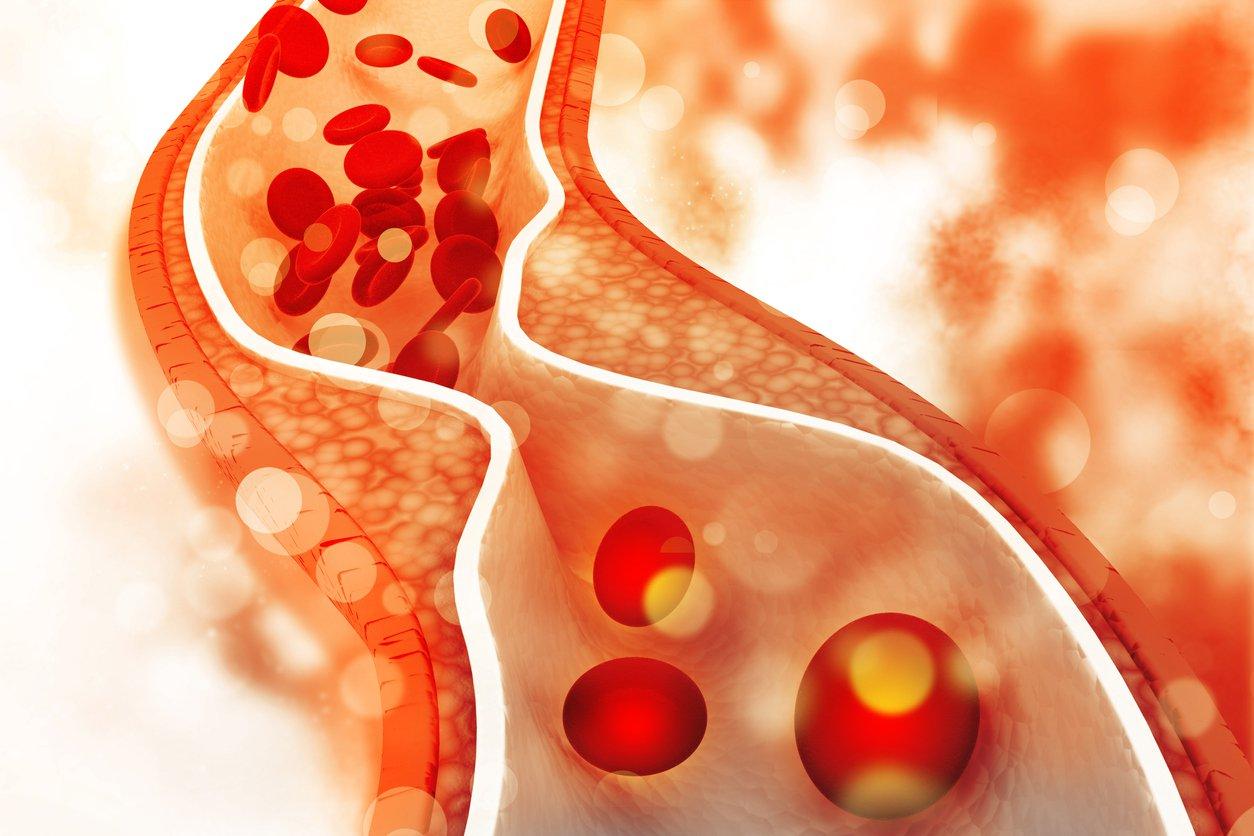
Triple vessel disease is an extreme form of coronary artery disease (CAD). CAD develops when the major blood vessels supplying the heart become damaged or diseased. Plaque (cholesterol deposits) and inflammation are the two main causes of CAD.
While minor plaque deposits may not impede the blood flow to the heart, larger plaque deposits may significantly decrease or even block the flow of blood to the heart. These blockages may cause a patient to experience chest pain, shortness of breath or even cause a heart attack.
While most CAD may only significantly impact one of the major coronary arteries, triple vessel disease, as the name implies, impacts the three major blood vessels that supply the heart with blood (left anterior descending, left circumflex, right coronary artery). The left ventricle also has reduced contractile function.
What is the prevalence of triple vessel disease?
It is estimated in the United States that half of the healthy 40-year-old men will develop CAD in the future, while 1 in 3 healthy 40-year-old women will develop CAD. While the studies vary, it is estimated that roughly 26-33% of all patients with CAD will develop triple vessel disease.
This equates to roughly 1 in 8 men and 1 in 12 women who will develop TVD in their lifetime. In the US, there are currently 40.9 million men and 27.2 million women who will be impacted by triple vessel disease during their lifetime.
What causes triple vessel disease?
Triple vessel disease is usually caused by atherosclerosis, hardening or clogging of the arteries. Atherosclerosis is caused by plaque, which is formed by cholesterol, calcium or fatty deposits within the inner walls of the arteries.
These plaques physically restrict or clog the arteries, resulting in reduced blood flow to the heart tissue and may have detrimental effects on the artery tone and function. Additionally, the reduced blood supply restricts the heart tissue from receiving the necessary amount of oxygen and vital nutrients needed to function properly. When the energy demands of the heart are not met by the incoming blood supply, a heart attack may occur.
Atherosclerosis can occur in any artery in the body, including other major organs. Pieces of the plaque may also break off, causing blood clots. If left untreated, the condition may lead to myocardial infarction or stroke.
Xem thêm : The 6 Best Pre-Workout with 400 mg Caffeine
While many things can potentially contribute to triple vessel disease, the most common risk factors are: Poor diet, obesity, lack of exercise, smoking, age, diabetes and hereditary factors.
What are the symptoms of triple vessel disease?
Symptoms of Triple Vessel Disease mirror those of CAD:
- Chest pain
- Shortness of breath
- Fatigue
- Confusion
- Heartburn or choking feeling
- Nausea or vomiting
- Pain or discomfort in the upper areas of the body, such as back, jaw, neck, arms or shoulders
- Dizziness or light-headedness
- Rapid or irregular heartbeat
Patients that have blockages in other arteries of the body may experience pain or muscle weakness in those areas too.
How is triple vessel disease detected?
There are a few key diagnostic tests that are performed in order to diagnose CAD and triple vessel disease. The most common are:
Electrocardiogram
An electrocardiogram, or ECG, is an exam that records the electrical signals as they travel throughout your heart. This may be performed in a hospital, outpatient setting or a patient may be equipped with a Holter monitor; a type of portable monitor that records the electrical signals for an extended period of time that the patient wears as they go about their normal, daily routine.
Echocardiogram
An echocardiogram is performed using an ultrasound machine. During the exam, the cardiac tissue is imaged and the physician is able to determine whether all parts of the heart are functioning correctly and if they are contributing normally to the heart’s pumping activity.
Stress test
If a patient experiences signs and symptoms of CAD most frequently during exercise, a stress test may be the recommended examination. During this exam, the patient will be asked to exercise (ride a stationary bike or walk on a treadmill) if they are able. If the patient is unable to exercise, a medication may be administered to simulate exercise.
Imaging, using a SPECT camera such as the Digirad Cardius C3 or X-ACT+, will be performed to determine what parts of the heart are receiving adequate blood flow during rest and stress in addition to other important information.
A stress test may be performed using an MRI or an ultrasound but is most commonly performed within nuclear medicine, often referred to as a nuclear stress test. Nuclear stress tests may be performed using gamma emitting radiation on a SPECT gamma camera or using positron-emitting radiation on a PET imaging system.
Cardiac catheterization and angiogram
An angiogram involves injecting a contrast dye into the coronary arteries through a long, thin, flexible tube called a catheter. This catheter is threaded through an artery, typically in the leg, all the way to the arteries in the heart.
While the physician is viewing the function and blood flow of the heart, they may choose to insert a balloon through the catheter. Once inflated, the balloon may improve blood flow through the heart where blockages and restricted blood flow was observed.
CT coronary angiogram
Xem thêm : How To Eat 200 Grams of Protein A Day: 5-Day Sample Meal Plans
A computed tomography (CT) examination of the heart may be beneficial to visualize calcium deposits within the arteries that restrict blood flow and may create blockages. During this exam, the physician may choose to utilize contrast to determine the blood flow throughout the vasculature of the heart.
What role does coronary flow reserve (CFR) play?
There has been much discussion surrounding the assessment of coronary flow reserve (CFR) in the diagnosis of triple vessel and coronary artery disease. Like other organs, auto-regulation is an important ability of the heart that is defined as “the ability of an organ to maintain a constant blood flow despite changes in perfusion pressure.” To determine the CFR, the ratio between resting and maximal possible coronary blood flow is calculated. The CFR can be thought of as the ability of the coronary circulation to dilate and increase flow following increased metabolic demands (exercise).
While the CFR data can help classify patients, it should not be relied upon as the only classification tool (low, intermediate, high risk for CAD). It is important to remember that CFR data is acquired in conjunction with PET imaging or in conjunction with a cardiac catheterization. These contributing factors may influence the conversation and the perceived importance of CFR versus what the actual CFR impact is on patient management.
It is also important to note that the ability of a reduced global CFR to predict multivessel (including TVD) CAD has not been promising. One study described a CFR of <1 as only yielding a 50% positive predictive value.
Another popular study found that the CFR data had a modest contribution in the ability to predicting high-risk CAD. There is a need for further investigation regarding the importance of CFR for the diagnosis in multivessel CAD; the current available studies indicate that the use of CFR in multivessel CAD is rather poor.
Can you just use a CCTA exam?
Some people ask if a CCTA exam will suffice as an all-in-one test for anatomical and perfusion-based imaging. While coronary computed tomography angiography (CCTA) has increased its prognostic abilities due to technological advances, it does not perform well enough on its own to replace traditional radionuclide (nuclear medicine) myocardial perfusion imaging. As a standalone, it falls short of being able to encompass both the anatomical and perfusion-based assessment as an all-in-one test.
Below is a simplified, proposed pathway for diagnosing CAD. As mentioned in the “Abnormal” imaging pathway, radionuclide imaging should be considered for indeterminant stenosis on CCTA. It is recommended to include radionuclide imaging as a standard imaging test for diagnosing CAD patients in addition to CMR or CCTA.
Treatment options for CAD and TVD
While treatment options vary based on the individual patient, provider and resources available, there are three main approaches taken to address CAD and TVD.
#1. Reduce the heart’s workload
- Controlling blood pressure and using certain drugs such as calcium channel blockers or beta-blockers
#2. Improve blood flow through the coronary arteries
- Pharmacologic intervention using drugs that promote the relaxation of the coronary arteries
- Invasive procedures such as: – Percutaneous coronary intervention (PCI) to stretch narrowed arteries – Coronary artery bypass grafting (CABG) to bypass the blockages
#3. Slow down or reverse the buildup of atherosclerosis or plaque
- Impacted by lifestyle changes such as modifying the diet, increased exercise and by taking certain medications
In summary…
While there have been many advances in technological capabilities, the prognostic capability of nuclear SPECT for triple vessel coronary artery disease is still the optimal route to go.
There is a lot of buzz and discussion surrounding coronary flow reserve and coronary computed tomography angiography, and the potential applications thereof. These procedures and the data obtained still need further investigation to determine their role in diagnosing CAD.
At this point in time, our belief is that providers should be cautious while evaluating these newer capabilities and technologies, while ensuring that their workups for CAD diagnostic imaging continue to include the tried and true capabilities of nuclear SPECT imaging.
Reimbursement Information
While all facilities and physicians have their standard order sets, these are the most commonly used CPT codes and national reimbursement rates used in conjunction with triple vessel coronary artery disease.
Nguồn: https://buycookiesonline.eu
Danh mục: Blog
This post was last modified on November 18, 2024 2:53 am