Calcium channel blockers are medications that help decrease blood pressure, prevent angina, and treat dysrhythmias. This review will discuss the mechanism of action of calcium channel blockers, what conditions they treat, nursing implications, side effects, and patient education.
Don’t forget to take the calcium channel blockers quiz after reviewing this material.
Bạn đang xem: Calcium Channel Blockers Nursing Pharmacology NCLEX Review
Calcium Channel Blockers Lecture
Calcium Channel Blockers Nursing Pharmacology Review
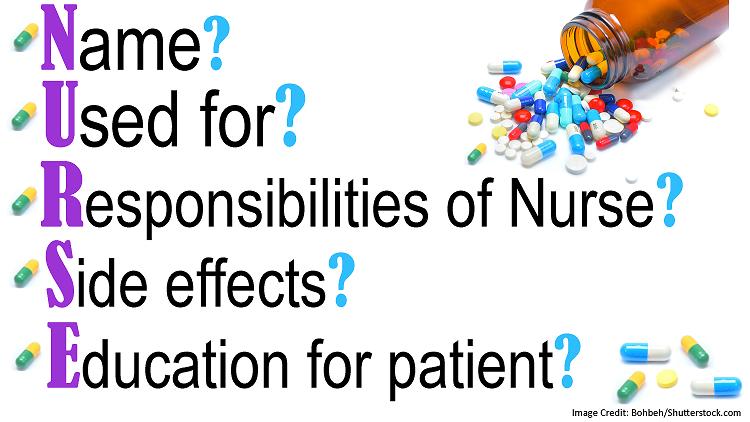
Always ask yourself these 5 questions when you see a drug name to help you understand how the drug works, your role as a nurse, and what information will be asked on an exam about the drug:
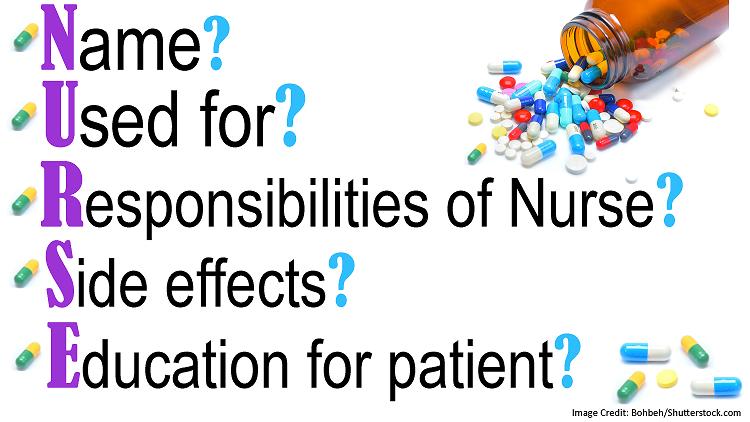
Name (specifically the family name)? This will tell how the drug works.
Used for? This will tell you WHY the drug was ordered…what condition is this medication treating in your patient?
Responsibilities as the nurse? This will tell you what your role is as the nurse and what you need to monitor in the patient.
Side effects? Know the common side effects of the medications
Xem thêm : Food truck growth in Illinois hits speed bumps
Education pieces for the patient? As the nurse we play a HUGE role in educating our patients on how to take the drug, what to watch out for, and when to call the doctor.
Now, using those 5 questions let’s go over what you need to know about calcium channel blockers for exam:
Name?
- Calcium channel blockers work to block the L-type calcium channels in the:
- Vascular smooth muscle cells: coronary arteries and peripheral arteries
- Cardiac myocytes: cells that control the strength of the heart’s contractions
- Cardiac nodal tissue: cells that are responsible for the electrical conduction of the heart (specifically the cells in the SA and AV nodes)
What’s the big deal about blocking calcium channels? Calcium plays a HUGE role in cell contraction. Therefore, if cell contraction can be decreased or inhibited it will cause cell relaxation. In some cases such as hypertension, angina, and certain types of dysrhythmias, it’s advantageous for the cell to relax rather than contract.
The key to truly understanding CCBs is to understand how they affect the calcium channels in the specific areas listed above. Once you grasp this, there is no need for memorization of the nursing implications, side effects, patient education, or what these medications are used for because it will make complete sense.
When calcium channels are blocked in the areas above this is what occurs in the body:
Vascular smooth muscle:
A calcium channel blocker will inhibit the calcium channels from opening and allowing calcium into the cell so contraction can’t occur. This will cause the vascular smooth muscle (we’re mainly talking about the coronary arteries and arteries…not veins) within the body to relax. This will cause:
- Vasodilation
- When peripheral arteries relax (hence vasodilate) this will decrease arterial blood pressure.
- This leads to a decrease in systemic vascular resistance (SVR) -> decreases cardiac afterload:
- Remember cardiac afterload is the amount of resistance the left ventricle must overcome to pump out blood. If we decrease that resistance (hence the SVR), it will ease the workload on the heart and decrease the oxygen consumption by the myocardium.
- Dilation of coronary arteries: the cardiac muscle will benefit from this because it will allow more blood to flow (hence oxygen) to the cardiac muscle. In addition, the dilation can help prevent a spasm of the coronary arteries because their relaxed.
- What these medications are great at treating?
- Hypertension and angina (especially variant angina “prinzmetal angina”
- Prinzmetal angina is chest pain that occurs at rest due to a vasospasm of the coronary arteries. CCBs will keep them relaxed.
- Hypertension and angina (especially variant angina “prinzmetal angina”
- What these medications are great at treating?
- This leads to a decrease in systemic vascular resistance (SVR) -> decreases cardiac afterload:
- When peripheral arteries relax (hence vasodilate) this will decrease arterial blood pressure.
Cardiac myocytes:
A CCB will prevent calcium from entering the cell of the cardiac myocytes. These cells control the strength of heart muscle contraction. Therefore, if we block the calcium channels from allowing calcium into the cell, contractions can’t occur and this will decrease the cardiac muscle cell’s strength of contraction.
- This provides a negative inotropic effect: this is beneficial because it will decrease the oxygen demand of the cardiac muscle (again why they’re great at treating/preventing angina especially the variant type).
- However, CCBs are NOT good for some patients with heart failure. WHY?
- Some patients will heart failure already has a heart muscle that is weak and can’t contract efficiently. If we put them on a CCB, this will further weaken the heart’s contractions….not good!
- However, CCBs are NOT good for some patients with heart failure. WHY?
Xem thêm : 3 Nephi 17
Cardiac nodal tissue:
A calcium channel blocker will prevent calcium channels within the SA and AV nodes from opening to allow calcium in, which will help nodal cells contract.
- If calcium channels are blocked in the SA (sinoatrial) node, this will DECREASE the heart rate (remember the SA node is the pacemaker).
- This produces a negative chronotropic effect.
- If calcium channels are blocked in the AV (atrioventricular) node, it will DECREASE the speed of conduction of the electrical impulses (remember the AV node is the gatekeeper and relays the electrical impulses by slowing down the impulse it received from the SA node).
- This produces a negative dromotropic effect.
- This is why *SOME CCBs are great at treating dysrhythmias like supraventricular tachycardia and atrial fibrillation. These dysrhythmias result in a fast, abnormal heart beat that usually starts in the AV node.
- This produces a negative dromotropic effect.
*There are different types of calcium channel blockers and some are more selective to the heart and provide more of an antiarrhythmic effect. Below are the types of CCBs.
Types of Calcium Channel Blockers
Dihydropyridines: end with “pine”
- Amlodipine
- Felodipine
- Nifedipine
- More vascular smooth muscle selective
- Mainly for hypertension and angina
Non-dihydropyridines: more myocardium selective
- Phenylalkylamines: (Verapamil)
- Benzothiazepines: (Diltiazem)
- Antiarrhythmic (helpful with supraventricular tachycardia and atrial fibrillation) , hypertension, angina
Used for?
Hypertension, angina, supraventricular tachycardia, a-fib, Raynaud’s disease (decreased circulation issues), spasms of vessels (cerebral), migraines, etc.
Responsibilities as the Nurse, Side effects, and Patient Education?
- Monitor vital signs, especially heart rate (bradycardia) and blood pressure (hypotension)
- Teach patient how to do this as well and to record it and report to the doctor if heart rate or blood is too low.
- Risk for reflex tachycardia due to hypotension (this occurs when the blood pressure drops and the heart rate increases to compensate for the decrease in blood pressure).
- Teach about orthostatic hypotension and that the patient needs to change positions slowly (this helps when there is a decrease in blood pressure when going from a sitting or lying position to a standing position).
- Monitor EKG closely for arrhythmias: 1st degree AV block is a side effect due to the decrease in the speed of conduction by the AV node.
- These medications are contraindicated in patients with 2 or 3rd degree heart block.
- Monitor for signs and symptoms of heart failure…WHY? Remember these medications (especially the non-dihydropyridines) alter how the heart pumps (creates a negative inotropic effect) and this weakens the heart’s contractions.
- Signs and symptoms of heart failure: crackles, edema, dyspnea, weight gain…monitor intake and output, daily weights, lung sounds etc.
- Teach patient to avoid taking CCBs with grapefruit juice….it will increase the drug level of the calcium channel blocker.
- Encourage a high fiber diet due to constipation with Verapamil or Diltiazem (these medications can slow down GI motility).
- Watch out for gingival hyperplasia: enlargement of gums….teach patient about good oral hygiene and regular dental visits (mainly with dihydropyridines ex: amlodipine)
Taking Digoxin too? Digoxin levels have to be monitored because CCBs can increase digoxin levels. Watch out for Digoxin toxicity…..signs and symptoms include (teach these signs and symptoms to the patient too):
- EARLY signs and symptoms are GI-related:
- Nausea, vomiting, anorexia
- Other signs and symptoms: vision changes with reports of yellow-greenish vision or halos, blurred vision and EKG changes….(dysrhythmias)…tends to be later on.
- Therapeutic range: 0.5 -2 ng/mL (greater than 2 ng/mL is toxic)
- Nausea, vomiting, anorexia
More Pharmacology Reviews
References
Nguồn: https://buycookiesonline.eu
Danh mục: Info