History & Epidemiology
Wolff Parkinson White syndrome, or WPW syndrome, is a condition that occurs when an extra electrical pathway in the heart causes a rapid heartbeat leading to congenital pre-excitation of the heart. In some cases, conduction through this accessory pathway leads to malignant tachyarrhythmias.1 In a normal heart, electricity is conducted from the atria to the ventricles through the atrioventricular (AV) node.1
The hallmark finding of Wolff Parkinson White syndrome is the electrocardiographic (ECG) finding of the delta wave.1 Many patients are asymptomatic making epidemiological tracking a challenge. The estimated prevalence of WPW syndrome in the general population is 0.1 to 0.3%.1
Bạn đang xem: Wolff Parkinson White Syndrome
Wolff Parkinson White Syndrome Diagnosis & Presentation
Because some Wolff Parkinson White syndrome patients never develop an arrhythmia, these patients may be asymptomatic and have a normal physical exam.1 Symptomatic patients typically present with cardiovascular symptoms such as palpitations, presyncope, or syncope due to tachyarrhythmia.2
Patients who are symptomatic may also present with chest pain, dyspnea, and even sudden cardiac death (SCD).1 SCD typically occurs due to ventricular fibrillation.
Patients who previously experienced arrhythmia may have learned of their condition if an ECG was performed and exhibited the hallmark delta wave ECG finding associated with Wolff Parkinson White syndrome.1 Patients may also discuss a family history of WPW syndrome.
Diagnostic Workup of Wolff Parkinson White Syndrome
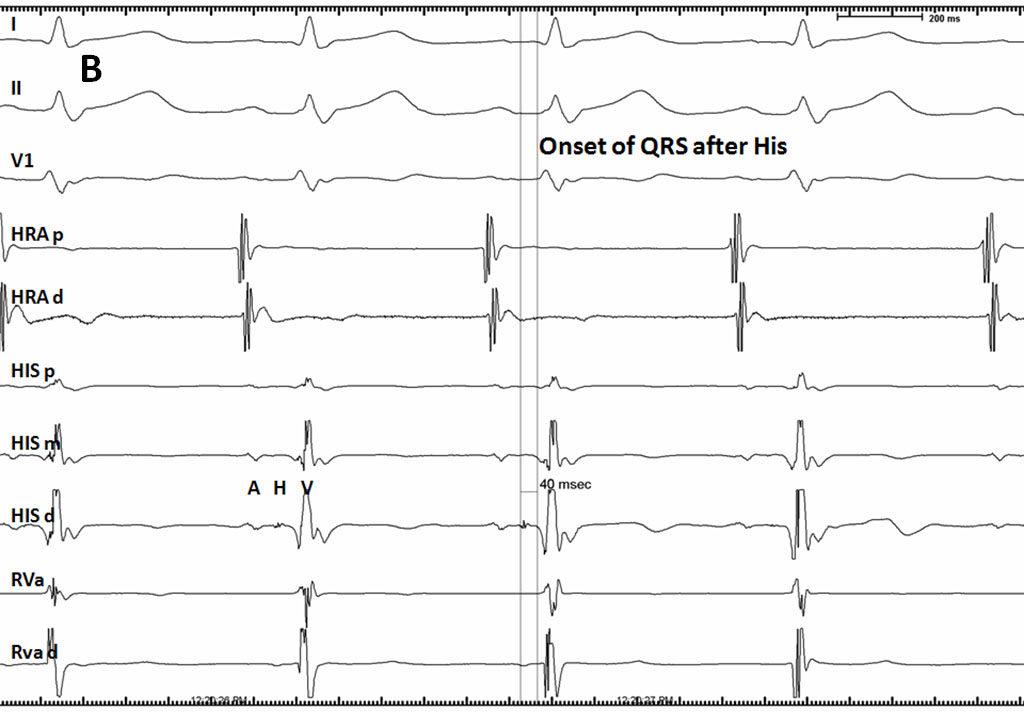
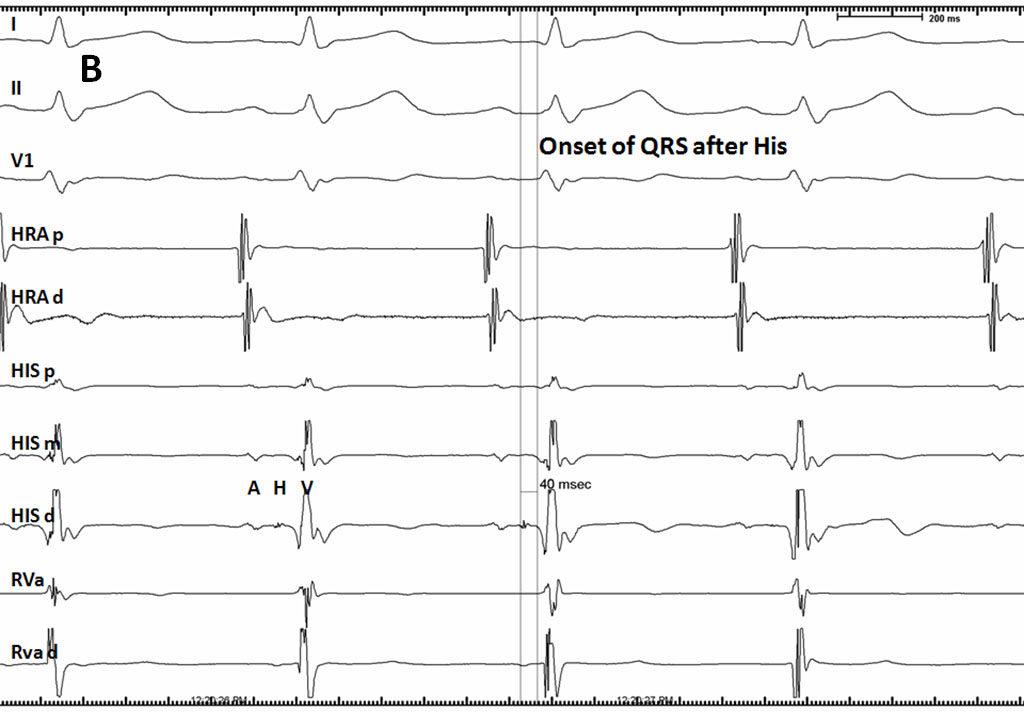
The initial diagnostic workup for Wolff Parkinson White syndrome includes the surface ECG.1 ECG findings that are associated with Wolff Parkinson White syndrome include a short PR interval (<120 ms), prolonged QRS complex (>120 ms), and QRS morphology that includes a slurred delta wave.1
WPW syndrome is split into type A and type B based on the direction of the dominant QRS deflection in lead V1 of the ECG.3 In Type A the QRS complex is typically upright with a negative delta wave in lead I.
In Type B the QRS complex and delta wave are typically negative in lead V1 while lead I shows a positive delta wave. Occasionally, patients may not present with this hallmark ECG pattern because some accessory pathway activity may be concealed.1
Further diagnostic workup may be done to identify higher risk patients, which are those patients who are at greater risk of SCD.1 Noninvasive methods for risk stratification include Holter monitoring, exercise treadmill testing, and echocardiography.2 When noninvasive testing is insufficient, electrophysiologic (EP) studies may also be performed.
WPW Syndrome Differential Diagnosis
The differential diagnosis for Wolff Parkinson White syndrome is broad and includes acute events such as myocardial infarction, structural disease such as congenital abnormality or hypertrophy, and other conduction abnormalities such as regular narrow complex tachycardia, irregular narrow complex tachycardia, and regular wide complex tachycardia.1
Management of Wolff Parkinson White Syndrome
Nonpharmacotherapy for WPW Syndrome
Wolff Parkinson White syndrome patients who are asymptomatic typically do not require immediate treatment.1 Evaluation by a cardiologist or electrophysiologist can help to identify higher risk, asymptomatic patients. These higher risk patients are candidates for catheter ablation of the accessory pathway and preventive antiarrhythmic treatment as further described below.
WPW syndrome patients who are symptomatic are typically treated with catheter ablation.1 Catheter ablation is the first-line treatment because it is less invasive than surgical ablation.
Pharmacotherapy for WPW Syndrome
Medical management is reserved for those who are poor candidates for catheter ablation and include flecainide and propafenone, among other medications.1
Patients with an acute episode of tachyarrhythmia are managed according to the 2010 American Heart Association guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care algorithm.1
Avoiding AV node blocking medications such as calcium channel blockers and beta blockers is essential as these medications can exacerbate symptoms.1
Monitoring Side Effects, Adverse Events, Drug-Drug Interactions
Xem thêm : Billing and Coding: Benign Skin Lesion Removal (Excludes Actinic Keratosis, and Mohs)
Catheter ablation procedures carry the risk of adverse events including the commonly cited AV block.4 Other serious complications include death, esophageal perforation, heart block requiring a pacemaker, stroke, phrenic nerve injury, and vascular access complications.5
Vascular access complications such as arteriovenous fistula, aneurysm, and retroperitoneal bleeding more commonly impact surgery recovery and occur in 2 to 4% of cases.5 Due to this broad range of possible complications, patients should be thoroughly informed of the risks prior to the procedure.
Medical management may include antiarrhythmic medications such as flecainide and propafenone. Both of these medications are part of the sodium channel blocker class 1C group of antiarrhythmic medications and therefore have similar profiles.6
When using for ventricular arrhythmia prophylaxis, flecainide dosage is 100 to 400 mg taken orally at 8 or 12-hour intervals.7 The dose may need to be adjusted for patients with renal disease.
Adverse Effects & Interactions
The main adverse effects are cardiac toxicity and an increased incidence of mortality which can occur due to the medication’s proarrhythmic effects. Flecainide is contraindicated with known hypersensitivity to flecainide, structural heart disease, and documented second or third-degree AV block, among others.7
The medication should be used with caution in patients who have myocardial dysfunction, heart failure, QT prolongation, electrolyte abnormalities, and those with a pacemaker. Flecainide interacts with many medications, and a thorough evaluation of drug-drug interactions should be performed with its use.
Significant interactions occur between flecainide and ritonovir, cisapride, despiramine, dronedarone, quinidine, saquinavir, and tipranavir.7
In addition to a sodium channel blocker profile, propafenone, also has beta blocking and calcium channel blocking activity which worsens its toxicity profile.6 As with flecainide, drug-drug interactions are common, and a thorough assessment of possible drug-drug interactions is necessary.
Patients with suspected sodium channel blocker toxicity should receive immediate ECG evaluation.6 Management of toxicity includes administration of sodium bicarbonate and management of hypotension, seizures, and extracorporeal membrane oxygenation (ECMO) in refractory cases.6
Drugs to avoid in Wolff Parkinson White syndrome are AV node blocking medications such as adenosine, calcium channel blockers, and beta blockers because these medications can exacerbate the associated arrhythmias.1
Read more: Beta Blockers in Heart Failure Management
Wolff Parkinson White Syndrome ICD 10 Code
Here is the ICD 10 code relevant to Wolff Parkinson White syndrome, or pre-excitation:
Frequently Asked Patient Questions
What are the symptoms of Wolff Parkinson White Syndrome?
Wolff Parkinson White (WPW) Syndrome is a condition characterized by rapid heartbeat, shortness of breath, chest pain, lightheadedness, fainting, palpitations – sensations of a beating or fluttering heart – as well as anxiety, fatigue and difficulty in breathing. In some cases, however, no symptoms are present.
Does Wolff Parkinson White syndrome shorten life expectancy?
Patients with WPW syndrome may experience a type of arrhythmia known as anterograde conduction over the accessory pathway when atrial flutter is present. Some of these pathways have shorter refractory periods than the AV node, which can lead to ventricular rates as high as 300 beats per minute. This rapid stimulation rate is not well tolerated and can result in ventricular fibrillation or cardiac arrest even in young, otherwise healthy individuals.
What does a Wolff Parkinson White ECG/EKG look like?
The WPW syndrome is a prime example of reentry. Generally, an electrical impulse created by the sinoatrial node (SA node) moves through atrial tissue to the atrioventricular node (AV node), which causes a slight delay before it reaches the ventricles. However, around 1% of people possess an additional connection between their atrium and ventricle known as an accessory pathway, or bypass tract, that allows conduction to skip over the AV node.
Xem thêm : Visitors
Because this route conducts impulses faster than normal, stimulation of the ventricles during sinus rhythm begins earlier than expected. In patients with WPW syndrome, the PR interval of the electrocardiogram is typically shorter than 0.12 seconds or 3 small boxes. This leads to a ventricular pre-excitation and an abnormally broadened QRS complex with a slurred initial upstroke, known as a delta wave.
Can Wolff Parkinson be cured?
Patients with WPW syndrome and accompanying arrhythmias are typically recommended to undergo an invasive electrophysiologic study with radiofrequency ablation of the accessory pathway. This process includes introducing a thin, pliable tube (catheter) into a blood vessel in the groin and up to the heart for pinpointing and eliminating the extra electrical pathway that is causing WPW syndrome. Ablation has been shown to be highly successful in curing this condition, however, there may be instances where repeat procedures or medical management through anti-arrhythmic medications may be necessary.
In the case of long-term oral medication, it is recommended to use drugs that impede conduction through accessory pathways (e.g. class IA, IC or III agents). Sodium channel blockers (class IA and IC antiarrhythmics) and certain class III antiarrhythmic medications are particularly effective in slowing down conduction as well as prolonging the refractory period of accessory pathways and atrioventricular node; thus, they are considered optimal for this particular condition.
What medications should be avoided by patients with Wolff Parkinson White syndrome?
Digitalis, beta blockers, and calcium channel blockers are effective in inhibiting conduction through the AV node; however, they do not impede conduction over most accessory pathways. On the contrary, these drugs may actually reduce the refractory period of an accessory pathway which could lead to a faster ventricular rate (and a risk of hemodynamic collapse) if administered to individuals suffering from WPW syndrome who experience atrial flutter.
What triggers Wolff Parkinson White syndrome?
Patients with WPW syndrome, a condition characterized by ventricular preexcitation, may experience atrial impulses that travel in an anterograde direction to the ventricles via both the AV node and an accessory pathway. Generally, conduction through the accessory pathway is faster than that of normal conduction over the AV node; thus leading to earlier stimulation of the ventricles.
References
1. Chhabra L, Goyal A, Benham MD. Wolff Parkinson White syndrome. In: StatPearls. NCBI Bookshelf version. StatPearls Publishing: 2022. Accessed July 14, 2022.
2. Rao AL, Salerno JC, Asif IM, Drezner JA. Evaluation and management of Wolff Parkinson White in athletes. Sports Health. 2014;6(4):326-332.
3. Narula OS. Wolff Parkinson White syndrome. Circulation. 1973;47:872-887.
4. Cohen M, Triedman J. Guidelines for management of asymptomatic ventricular pre-excitation. Circ Arrhythm and Electrophysiol. 2014;7(2):187-189. doi:10.1161/CIRCEP.114.001528.
5. Ghzally Y, Ahmed I, Gerasimon G. Catheter ablation. In StatPearls. NCBI Bookshelf version. StatPearls Publishing: 2021. Accessed July 14, 2022.
6. Dokken K, Fairley P. Sodium channel blocker toxicity. In StatPearls. NCBI Bookshelf version. StatPearls Publishing: 2022. Accessed July 14, 2022.
7. Arunachalam K, Alzahrani T. Flecainide. In StatPearls. NCBI Bookshelf version. StatPearls Publishing: 2021. Accessed July 14, 2022.
Author Bio
Anna Courant is a nurse practitioner and writer.
Updated: 11/16/2023
Nguồn: https://buycookiesonline.eu
Danh mục: Info