What Is a Hysteroscopy?
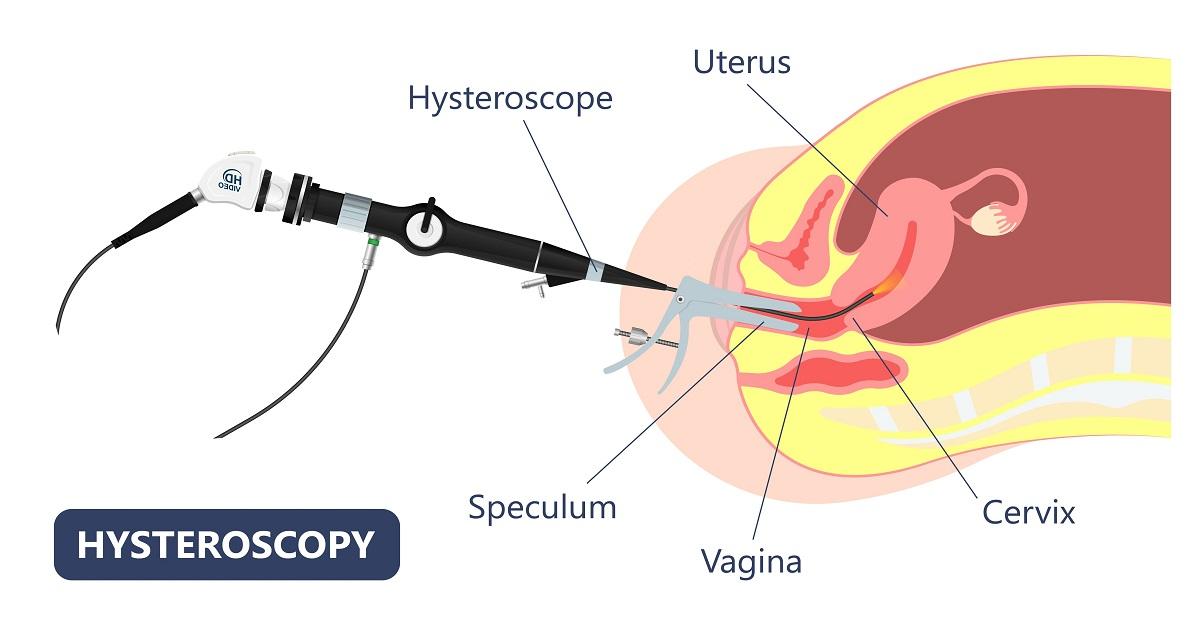
Hysteroscopy is a medical procedure that allows doctors to view the inside of a woman’s uterus using a thin, lighted tube called a hysteroscope. It is typically used for diagnostic and operative purposes. Hysteroscopy in IVF is a treatment process which is explained further.
Diagnostic Hysteroscopy:
Diagnostic hysteroscopy is used to identify the cause of abnormal uterine bleeding, infertility, and other reproductive health issues. The procedure involves inserting a hysteroscope into the vagina and through the cervix into the uterus. A camera attached to the hysteroscope sends images of the uterus to a monitor, allowing the doctor to examine the uterine lining, fallopian tubes, and other structures for any abnormalities. Diagnostic hysteroscopy is typically performed in an office or outpatient setting and is generally well-tolerated by patients.
Bạn đang xem: What is the Role of Hysteroscopy in IVF?
Operative Hysteroscopy:
Operative hysteroscopy is used to treat various uterine conditions, such as fibroids, polyps, and adhesions. It is similar to diagnostic hysteroscopy in that a hysteroscope is inserted into the uterus, but in operative hysteroscopy, surgical instruments are also used to remove or treat any identified abnormalities. Operative hysteroscopy is usually performed under anaesthesia in a hospital or outpatient surgical centre.
What is Hysteroscopy done for?
Hysteroscopy is a medical procedure used to examine the inside of the uterus. It involves inserting a thin, flexible instrument called a hysteroscope through the vagina and cervix into the uterus. The hysteroscope is equipped with a light and camera, which allows the doctor to view the inside of the uterus and identify any abnormalities. Hysteroscopy may be done for various reasons, including:
- Unexplained vaginal bleeding: Hysteroscopy can help identify the cause of abnormal vaginal bleeding, such as heavy periods, bleeding between periods, or bleeding after menopause.
- Infertility: Hysteroscopy can help identify and treat conditions that may affect fertility, such as uterine fibroids, adhesions, or polyps.
- Recurrent miscarriage: Hysteroscopy can help identify and treat conditions that may contribute to recurrent miscarriage, such as a uterine septum or adhesions.
- Abnormal Pap test: Hysteroscopy can help identify and treat abnormal cells or growths in the cervix or uterus.
- Pelvic pain: Hysteroscopy can help identify and treat conditions that may cause pelvic pain, such as endometriosis or uterine fibroids.
- IUD placement: Hysteroscopy can be used to guide the placement of an intrauterine device (IUD) for birth control.
Overall, hysteroscopy is a safe and effective procedure that can help diagnose and treat a range of gynaecological conditions. It is typically performed as an outpatient procedure and does not require a hospital stay. Your doctor can help determine if hysteroscopy is the right option for you based on your individual symptoms and medical history.
What is the Role of Hysteroscopy in IVF?
Hysteroscopy can also be used in conjunction with in-vitro fertilization (IVF) to increase the chances of successful embryo implantation. Before beginning IVF, a woman may undergo a hysteroscopy to assess the uterine cavity and determine if there are any uterine abnormalities that could affect implantation. If any abnormalities are identified, they can be treated during the same procedure, increasing the likelihood of a successful outcome.
In conclusion, hysteroscopy is a valuable tool in diagnosing and treating various uterine conditions. Whether used for diagnostic or operative purposes, hysteroscopy is generally a safe and well-tolerated procedure that can provide important information about a woman’s reproductive health. When used in conjunction with IVF, hysteroscopy can increase the chances of a successful pregnancy outcome.
Why Hysteroscopy Performed before IVF?
Hysteroscopy is a diagnostic and therapeutic procedure that involves the insertion of a thin, lighted tube called a hysteroscope into the vagina and through the cervix to examine the inside of the uterus. It is an important step before in-vitro fertilization (IVF) as it can help identify and treat any uterine abnormalities that may affect the success of the IVF procedure.
Here are some reasons why hysteroscopy is recommended before IVF:
- Identification of uterine abnormalities: Hysteroscopy can help identify various uterine abnormalities such as fibroids, polyps, adhesions, and septums that may interfere with implantation, decrease pregnancy rates, or increase the risk of miscarriage. By detecting these abnormalities, the chances of a successful pregnancy can be improved by treating or removing them before starting IVF treatment.
- Evaluation of the uterine cavity: Hysteroscopy can provide a clear view of the uterine cavity and help assess its size, shape, and orientation. Any abnormalities that may prevent successful embryo transfer or reduce the chances of implantation can be identified and treated before starting IVF.
- Improved accuracy of embryo transfer: Hysteroscopy can help ensure the correct placement of embryos during the transfer process. It allows the doctor to accurately place the embryos in the most favourable location in the uterus, thus increasing the chances of successful implantation and pregnancy.
- Improvement in IVF success rates: Studies have shown that hysteroscopy before IVF can improve pregnancy rates and reduce the risk of miscarriage. By detecting and treating any uterine abnormalities, the chances of successful implantation and pregnancy are increased.
Time Between Hysteroscopy & IVF;
The ideal time between hysteroscopy and IVF varies depending on the individual case and the severity of any uterine abnormalities found during the procedure. In general, it is recommended to wait for at least one to two menstrual cycles before starting IVF after hysteroscopy to allow the uterus to heal and to maximize the chances of success.
Procedure of Hysteroscopy:
Hysteroscopy is a minimally invasive procedure that allows a doctor to examine the inside of a woman’s uterus using a thin, lighted tube called a hysteroscope. The procedure can be done on an outpatient basis, under local anaesthesia or sedation.
- The first step in a hysteroscopy is to dilate the cervix to allow the hysteroscope to pass through. This is typically done with the use of a series of dilators, which gradually widen the cervix.
- Once the cervix is dilated, the hysteroscope is inserted through the vagina and into the uterus. The hysteroscope contains a light source and a camera that sends images to a monitor, allowing the doctor to see the inside of the uterus.
- During a diagnostic hysteroscopy, the doctor will look for any abnormalities such as polyps, fibroids, or adhesions. If an abnormality is identified, the doctor may take a biopsy or remove the abnormal tissue using surgical instruments.
- During operative hysteroscopy, the doctor may use specialized surgical instruments to remove or treat any identified abnormalities in the uterus.
- After the procedure is complete, the hysteroscope is removed, and the cervix is allowed to close naturally. Patients may experience some cramping or light bleeding for a few days after the procedure.
Benefits of Hysteroscopy:
Hysteroscopy has several benefits over traditional surgical procedures. Because it is minimally invasive, it typically results in less pain and scarring than traditional surgery. It also has a shorter recovery time, allowing patients to return to their normal activities sooner.
Hysteroscopy is a medical procedure that allows a doctor to examine the inside of the uterus using a thin, lighted instrument called a hysteroscope. Here are some benefits of hysteroscopy:
- Accurate diagnosis: Hysteroscopy allows doctors to accurately diagnose and treat various uterine conditions, such as abnormal uterine bleeding, fibroids, polyps, adhesions, and uterine septum.
- Minimally invasive: Hysteroscopy is a minimally invasive procedure that does not require incisions. It is performed as an outpatient procedure, which means patients can go home on the same day of the procedure.
- Improved treatment outcomes: Hysteroscopy allows doctors to perform certain surgical procedures inside the uterus, such as removing fibroids or polyps, correcting uterine septum, and removing adhesions. This can lead to improved treatment outcomes, reduced pain, and faster recovery.
- Improved fertility: Hysteroscopy can improve fertility in women by correcting structural abnormalities in the uterus and removing any obstructive growths.
- Fewer complications: Hysteroscopy has fewer complications than traditional open surgery, such as reduced blood loss, infection, and scarring.
Risks of Hysteroscopy:
Like any medical procedure, hysteroscopy comes with some risks. Here are some potential risks of hysteroscopy:
- Bleeding: Some women may experience mild bleeding after the procedure.
- Infection: Hysteroscopy can introduce bacteria into the uterus, which can lead to infection.
- Perforation: In rare cases, the hysteroscope can accidentally perforate the uterus or cervix, which can lead to bleeding or infection.
- Anaesthesia risks: Hysteroscopy requires anaesthesia, which carries some risks, such as allergic reactions and breathing difficulties.
- Postoperative pain: Some women may experience mild to moderate cramping or discomfort after the procedure.
It’s important to note that the risks of hysteroscopy are relatively low, and the benefits generally outweigh the risks. Women should talk to their doctor about their specific risks and any concerns they may have.
Hysteroscopy Cost in India:
The cost of hysteroscopy in India can vary depending on a number of factors, such as the location, the hospital or clinic, and the specific procedure being performed. Here are some approximate costs for hysteroscopy in India:
- Diagnostic hysteroscopy: Rs. 10,000 to Rs. 30,000
- Operative hysteroscopy: Rs. 25,000 to Rs. 75,000
These costs may or may not include additional fees for anaesthesia, medications, and hospital charges. Patients should talk to their doctor or hospital about the total cost of the procedure and any available payment options or insurance coverage. It’s important to note that some insurance companies may cover the cost of hysteroscopy, depending on the patient’s policy and the specific procedure being performed.
When to Avoid Hysteroscopy:
While hysteroscopy is a relatively safe and effective procedure, there are certain circumstances in which it may not be recommended. Here are some instances when hysteroscopy should be avoided:
- Pregnancy: Hysteroscopy is generally not recommended during pregnancy, as it may increase the risk of miscarriage or premature labour.
- Active infection: If a woman has an active infection, such as pelvic inflammatory disease (PID), hysteroscopy may not be recommended due to the risk of spreading the infection.
- Uncontrolled bleeding: If a woman is experiencing uncontrolled bleeding, such as heavy menstrual bleeding or bleeding disorders, hysteroscopy may not be recommended until the bleeding is under control.
- Cervical cancer: If a woman has cervical cancer or is at high risk for cervical cancer, hysteroscopy may not be recommended due to the risk of spreading cancer.
Heart or lung disease: If a woman has severe heart or lung disease, hysteroscopy may not be recommended due to the risks associated with anaesthesia.
Who Needs a Hysteroscopy:
Hysteroscopy may be recommended for women who are experiencing certain symptoms or conditions related to the uterus. Here are some instances when a woman may need a hysteroscopy:
- Abnormal uterine bleeding: Hysteroscopy may be recommended to evaluate the cause of abnormal uterine bleeding, such as heavy or prolonged menstrual bleeding, bleeding between periods, or bleeding after menopause.
- Infertility: Hysteroscopy may be recommended to evaluate the uterus for any structural abnormalities that may be impacting fertility.
- Fibroids or polyps: Hysteroscopy may be recommended to remove fibroids or polyps from the uterus.
- Adhesions or scar tissue: Hysteroscopy may be recommended to remove adhesions or scar tissue that may be causing pain or infertility.
- Uterine septum: Hysteroscopy may be recommended to correct a uterine septum, which is a congenital condition where the uterus is divided by a wall of tissue.
When Should a Hysteroscopy be Done:
The timing of a hysteroscopy depends on the reason for the procedure. Here are some instances when a hysteroscopy may be done:
- Diagnostic hysteroscopy: A diagnostic hysteroscopy may be done during the first half of a woman’s menstrual cycle, typically between days 6 and 10.
- Operative hysteroscopy: An operative hysteroscopy may be done after a diagnostic hysteroscopy if a problem is identified that requires surgery. The timing of the surgery will depend on the specific problem being addressed.
- Hysteroscopy for fertility: If hysteroscopy is being done to evaluate the uterus for fertility issues, it may be done during the first half of a woman’s menstrual cycle, typically between days 6 and 10.
- Hysteroscopy for postmenopausal bleeding: If hysteroscopy is being done to evaluate the cause of postmenopausal bleeding, it should be done as soon as possible to rule out the possibility of cancer.
Hysteroscopy Vs. Laparoscopy:
Hysteroscopy and laparoscopy are both diagnostic procedures used to evaluate reproductive organs, but they differ in the area of examination.
Hysteroscopy is used to examine the inside of the uterus and is performed through the vagina and cervix. A hysteroscopy is used to view the uterine cavity, detect abnormalities, and perform certain surgical procedures if needed.
Laparoscopy, on the other hand, is a procedure that examines the outside of the uterus, including the ovaries, fallopian tubes, and pelvis. It involves the insertion of a laparoscope, a thin, lighted tube, through a small incision in the abdomen to view the reproductive organs.
While both procedures can help diagnose and treat infertility, the choice between hysteroscopy and laparoscopy depends on the specific condition being evaluated. Hysteroscopy is typically used to diagnose and treat uterine abnormalities, while laparoscopy is used to diagnose and treat conditions such as endometriosis, ovarian cysts, and tubal blockages.
In conclusion, hysteroscopy is an important step before IVF as it can help identify and treat any uterine abnormalities that may interfere with the success of the procedure. It is a safe and minimally invasive procedure that can improve the chances of successful implantation and pregnancy. The ideal time between hysteroscopy and IVF varies depending on the individual case, and the choice between hysteroscopy and laparoscopy depends on the specific condition being evaluated.
What To Expect at A Hysteroscopy:
Hysteroscopy is a minimally invasive procedure that is typically performed in an outpatient setting:
- Preparation: Before the procedure, you will be asked to empty your bladder and change into a gown. You may also be given medication to help you relax or manage any discomfort during the procedure.
- Anaesthesia: Local anaesthesia may be administered to the cervix to help numb the area and reduce discomfort during the procedure. In some cases, general anaesthesia may be used if the procedure is more complex or if the patient requests it.
- Insertion of the hysteroscope: The hysteroscope, a thin, lighted tube, will be inserted through the vagina and into the cervix. Carbon dioxide gas or saline solution may be used to expand the uterus and improve visibility during the procedure.
- Visual examination: Once the hysteroscope is inserted, the doctor will examine the uterine cavity and identify any abnormalities. If necessary, surgical instruments may be used to remove or treat any abnormal tissue.
- Recovery: After the procedure, you will be monitored for a short period to ensure that there are no complications. You may experience some mild cramping or spotting, but this should subside within a few days.
- Follow-up: Your doctor will discuss the results of the procedure with you and may recommend additional testing or treatment if necessary.
Does a Hysteroscopy Hurt?
Hysteroscopy is generally well-tolerated and causes minimal discomfort. However, some women may experience mild to moderate cramping or discomfort during the procedure. Here are some factors that may affect the level of discomfort during a hysteroscopy:
- Anaesthesia: The use of local anaesthesia can help reduce discomfort during the procedure. In some cases, general anaesthesia may be used if the procedure is more complex or if the patient requests it.
- Cervical stenosis: If the cervix is narrow or stenotic, it may be more difficult to insert the hysteroscope and may cause some discomfort.
- Patient anxiety: Anxiety or fear of the procedure can increase the perception of pain or discomfort. Your doctor can provide medication or other measures to help manage anxiety during the procedure.
- Duration of the procedure: A longer procedure may cause more discomfort than a shorter one. Most hysteroscopies take between 20 and 30 minutes to complete.
If you experience severe or persistent pain during or after the procedure, contact your doctor immediately.
How Long Does a Hysteroscopy Take?
The duration of a hysteroscopy depends on several factors, including the complexity of the procedure, the skill of the doctor, and any additional treatment that may be needed. Here are some factors that may affect the duration of a hysteroscopy:
- Type of hysteroscopy: Diagnostic hysteroscopy, which is used to examine the uterus, typically takes between 10 and 30 minutes to complete. Operative hysteroscopy, which is used to treat uterine abnormalities, may take longer depending on the type and extent of treatment needed.
- Experience of the doctor: A skilled and experienced doctor can perform the procedure more efficiently and accurately, reducing the time needed for the procedure.
- Additional treatment: If any uterine abnormalities are identified during the procedure, additional treatment may be needed, which can increase the duration of the procedure.
Xem thêm : All About Sushi & The Low FODMAP Diet
In general, most hysteroscopies take between 20 and 30 minutes to complete. After the procedure, you will be monitored for a short period to ensure that there are no complications, and you will be able to go home the same day
Can I Still Have a Hysteroscopy on My Period Cycle?
Yes, you can still have a hysteroscopy while on your period, but it may be more uncomfortable due to the increased sensitivity of the cervix during menstruation.
- Increased discomfort: The cervix may be more sensitive during menstruation, which can increase the discomfort of the procedure. Your doctor may recommend taking pain medication before the procedure or using local anaesthesia to help manage the discomfort.
- Reduced visibility: Blood and debris from the menstrual cycle can make it more difficult to see the uterus during the procedure. Your doctor may use a special instrument called a uterine sound to help guide the hysteroscope into the uterus and improve visibility.
- Increased risk of infection: There is a slightly increased risk of infection during menstruation due to the presence of blood in the uterus. Your doctor may recommend taking antibiotics before the procedure to reduce the risk of infection.
It is important to discuss any concerns or questions you may have with your doctor before the procedure.
Hysteroscopy Recovery:
After a hysteroscopy, most women are able to resume their normal activities within a day or two:
- Cramping: Mild to moderate cramping is common after a hysteroscopy, especially if any tissue or growths were removed during the procedure. Over-the-counter pain medication, such as ibuprofen or acetaminophen, can help manage the discomfort.
- Spotting: Light spotting or discharge may occur for a few days after the procedure. Using pads instead of tampons can help reduce the risk of infection.
- Rest and relaxation: It is important to take it easy for the first few days after the procedure to allow your body to heal. Avoid sexual activity, strenuous exercise and heavy lifting.
- Follow-up: Your doctor will schedule a follow-up appointment to discuss the results of the procedure and any additional treatment that may be needed.
Pain after Hysteroscopy:
Some women may experience pain or discomfort after a hysteroscopy. Here are some possible causes and ways to manage the pain:
- Cramping: Mild to moderate cramping is common after a hysteroscopy, especially if any tissue or growths were removed during the procedure. Over-the-counter pain medication, such as ibuprofen or acetaminophen, can help manage the discomfort.
- Infection: In rare cases, an infection may develop after a hysteroscopy, causing pain or fever. Contact your doctor immediately if you experience severe pain, fever, or chills after the procedure.
- Trauma or injury: In rare cases, the hysteroscope or surgical instruments used during the procedure may cause injury or trauma to the uterus, leading to pain or discomfort. Contact your doctor immediately if you experience severe or persistent pain after the procedure.
It is important to follow your doctor’s instructions for post-procedure care and to contact them immediately if you experience any severe or concerning symptoms.
FAQ:
Q: Is hysteroscopy a major surgery?
A: Hysteroscopy is generally considered a minimally invasive procedure and not a major surgery. It is done using a thin, flexible scope called a hysteroscope that is inserted through the cervix into the uterus to view the inside of the uterus.
Q: Can U Get Pregnant After hysteroscopy?
A: Yes, it is possible to get pregnant after a hysteroscopy. In fact, some women who have had trouble conceiving may benefit from a hysteroscopy to identify and treat any uterine issues that may be contributing to infertility.
Q: How long does it take to recover from a hysteroscopy?
A: The recovery time for a hysteroscopy is typically minimal. Many women can return to their normal activities the same day or the day after the procedure. However, some women may experience cramping, bleeding, or discharge for a few days after the procedure.
Q: Is hysteroscopy very painful?
A: Hysteroscopy can cause some discomfort or pain, but it is generally considered to be a tolerable procedure. Women may experience cramping, pressure, or a sensation of fullness during the procedure, but pain medication can be given to help manage any discomfort.
Q: On which day of period hysteroscopy is done?
A: The best time to perform a hysteroscopy is typically during the first half of a woman’s menstrual cycle, between days 5 and 14. This is because the lining of the uterus is thinner during this time, making it easier to view the inside of the uterus with the hysteroscope.
Q: How much does hysteroscopy cost in India?
A: The cost of a hysteroscopy in India can vary depending on several factors, including the location of the procedure, the type of anesthesia used, and any additional tests or treatments that may be required. On average, the cost of a hysteroscopy in India can range from 10,000 to 50,000 rupees.
Q: Is there any stitches in hysteroscopy?
A: Hysteroscopy is a minimally invasive procedure that typically does not require any stitches. The hysteroscope is inserted through the cervix and into the uterus, so there is no incision made in the abdomen or uterus that would require stitches.
Q: What are the risks of hysteroscopy?
A: Hysteroscopy is generally considered a safe procedure, but as with any medical procedure, there are some risks involved. Some possible risks of hysteroscopy include bleeding, infection, injury to the uterus or cervix, and reaction to anaesthesia.
Q: What is the cost of hysteroscopy?
A: The cost of a hysteroscopy can vary depending on several factors, including the location of the procedure, the type of anaesthesia used, and any additional tests or treatments that may be required. In general, the cost of a hysteroscopy in the United States can range from $1,000 to $5,000, although insurance may cover some or all of the cost.
Q: Can hysteroscopy treat infertility?
A: Hysteroscopy can be used to diagnose and treat certain conditions that may be contributing to infertility, such as uterine polyps, fibroids, or adhesions. By removing these obstructions, hysteroscopy can improve the chances of successful pregnancy.
Q: When is the best time to do hysteroscopy?
A: The best time to perform a hysteroscopy is typically during the first half of a woman’s menstrual cycle, between days 5 and 14. This is because the lining of the uterus during this time is thinner, making it easier to visualize the inside of the uterus with the hysteroscope. However, the timing of the hysteroscopy may also depend on the reason for the procedure and the individual’s specific circumstances.
Q: How successful is a hysteroscopy?
A: The success of a hysteroscopy depends on the reason for the procedure and the individual’s specific circumstances. In general, hysteroscopy is a safe and effective procedure for diagnosing and treating certain conditions that affect the uterus, such as polyps, fibroids, and adhesions. Studies have shown that hysteroscopy can improve the chances of successful pregnancy in some cases. However, the success of the procedure also depends on other factors, such as the individual’s overall health and fertility.
Q: Is hysteroscopy painful with Anaesthesia?
A: Hysteroscopy is generally not painful when performed under anaesthesia. The anaesthesia can be administered through a numbing injection or through a sedative given through an IV line. This can help minimize any discomfort or pain during the procedure.
Xem thêm : Fort Hunter Liggett
Q: Why hysteroscopy is done before IVF?
A: Hysteroscopy is often performed before IVF to evaluate the uterus for any abnormalities that may affect the success of the IVF procedure. This may include polyps, fibroids, adhesions, or other structural issues that could interfere with embryo implantation.
Q: Does hysteroscopy improve IVF success?
A: Hysteroscopy can improve the chances of success with IVF by identifying and treating any uterine abnormalities that may be contributing to infertility. By removing these obstructions, hysteroscopy can improve the chances of successful embryo implantation and pregnancy.
Q: Is hysteroscopy needed for IVF?
A: While hysteroscopy is not always required before IVF, it is often recommended as a routine part of the evaluation process. This can help identify any uterine abnormalities that may affect the success of the IVF procedure and allow for appropriate treatment before beginning the IVF process.
Q: How long after hysteroscopy can you do IVF?
A: The timing of IVF after hysteroscopy may vary depending on individual circumstances and the reason for the hysteroscopy. In general, it is recommended to wait at least one to two menstrual cycles after hysteroscopy before beginning IVF to allow for any healing or recovery.
Q: How long after hysteroscopy is frozen embryo transfer?
A: The timing of frozen embryo transfer after hysteroscopy may vary depending on individual circumstances and the reason for the hysteroscopy. In general, it is recommended to wait at least one menstrual cycle after hysteroscopy before attempting a frozen embryo transfer to allow for any healing or recovery.
Q: Is it easy to get pregnant after hysteroscopy?
A: Hysteroscopy can improve the chances of successful pregnancy by identifying and treating any uterine abnormalities that may be contributing to infertility. However, the ability to get pregnant after hysteroscopy may also depend on other factors, such as the individual’s overall health and fertility.
Q: Can U Get Pregnant After hysteroscopy?
A: Yes, it is possible to get pregnant after hysteroscopy. In fact, hysteroscopy can improve the chances of successful pregnancy by identifying and treating any uterine abnormalities that may be contributing to infertility.
Q: Is a hysteroscopy painful IVF?
A: Hysteroscopy is generally not painful when performed under anaesthesia, and it can be a helpful tool in improving the success of IVF by identifying and treating any uterine abnormalities that may be affecting fertility.
Q: How do I prepare my uterus for IVF?
A: There are several steps that can be taken to prepare the uterus for IVF, including optimizing overall health through diet and exercise, taking fertility medications to stimulate egg production, and undergoing procedures such as hysteroscopy to identify and treat any uterine abnormalities that may affect the success of the IVF procedure. Your doctor will provide specific guidance on preparing for IVF based on your individual circumstances.
Q: Do I need to rest after hysteroscopy?
A: It is recommended to rest for the first 24-48 hours after hysteroscopy to allow for any potential side effects, such as cramping or spotting, to subside. It is also important to avoid strenuous activity or exercise during this time.
Q: What is the next step after hysteroscopy?
A: The next step after hysteroscopy will depend on the reason for the procedure and the findings during the exam. If any uterine abnormalities were identified, further treatment may be recommended, such as medication or surgery. If no issues were found, the patient may resume normal activities.
Q: How painful is a hysteroscopy?
A: Hysteroscopy is generally not painful when performed under anaesthesia. Some women may experience mild discomfort or cramping during or after the procedure, but this can usually be managed with over-the-counter pain relievers.
Q: How many days do you bleed after hysteroscopy?
A: Bleeding after hysteroscopy is usually minimal and may last for a few days. Some women may experience light spotting for up to a week after the procedure.
Q: How long is recovery time from hysteroscopy?
A: Recovery time from hysteroscopy is typically one to two days, although this can vary depending on individual circumstances and the extent of the procedure. Most women are able to resume normal activities within a day or two after the procedure.
Q: On what day is frozen embryo transfer done?
A: The timing of frozen embryo transfer can vary depending on individual circumstances and the specific protocol being followed. In general, the transfer is typically done during the “window of implantation,” which is typically 5-7 days after ovulation or 3-5 days after blastocyst formation.
Q: What is the role of hysteroscopy in infertility?
A: Hysteroscopy can play an important role in diagnosing and treating the underlying causes of infertility, particularly in cases where uterine abnormalities may be contributing to fertility issues. By identifying and treating these issues, hysteroscopy can improve the chances of successful pregnancy and live birth.
Nguồn: https://buycookiesonline.eu
Danh mục: Info
This post was last modified on December 6, 2024 5:36 am